In this week’s issue of The Savvy Diabetic:
-
- Cooking DOES NOT Replace Insulin
- One Size Does Not Fit All: ex-Specific Precision Medicine in D Technology
- Clinical Trial for Oral Hypoglycemia Medication: Cadisegliatin
- Fat Cells “Remember” Obesity Even After Weight Loss
- Loneliness is as Deadly as Obesity and Smoking a Pack of Cigarettes a Day
- TSA Warns of “Juice-Jacking” of Smartphones, Devices at Airports
- Clinical Trial for Oral Insulin: Tregopil
- CVS/Cigna Sue Arkansas Re New PBM Law
- Call Centers Being Replaced by AI
Misinformation Alert: Cooking Does Not Replace Insulin Kelly Dawes on LinkedIn.com, 28 May 2025.
 A recent statement by Dr. Marty Makary suggesting that “cooking at home could replace insulin” is not only misleading, it’s dangerous and harmful to millions of people living with diabetes. Statements like this fuel stigma and spread misinformation that can have real-life consequences. Here’s the truth:
A recent statement by Dr. Marty Makary suggesting that “cooking at home could replace insulin” is not only misleading, it’s dangerous and harmful to millions of people living with diabetes. Statements like this fuel stigma and spread misinformation that can have real-life consequences. Here’s the truth:
-
-
- For people with Type 1 Diabetes, insulin is absolutely essential for survival. The body no longer produces it, no amount of cooking, exercise, or lifestyle changes can change that.
- Many people with Type 2 Diabetes also require insulin to manage blood glucose levels and prevent serious complications. It is not a failure, it’s a medical necessity.
-
When public figures minimize these realities, it:
-
-
- Spreads harmful myths
- Fuels shame and stigma
- Undermines the complexity of diabetes care
- Distracts from urgent issues like insulin access and affordability
-
We need compassion, accuracy, and respect, not dangerous simplifications. Let’s raise our voices to challenge stigma and champion facts. People with diabetes deserve better.
Read more: Misinformation Alert: Cooking Does Not Replace Insulin
One Size Does Not Fit All: The Need for Sex-Specific Precision Medicine in Diabetes Technology, a new research study published on Journals.safepub.com, 25 May 2025.
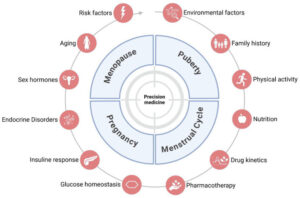 Incorporating sex-specific factors in diabetes research and treatment is essential for advancing precision medicine. There are critical gaps in understanding and applying sex-related differences. Female-specific diabetes pathophysiology manifests in three major areas: life cycle phases (including puberty, pregnancy, and menopause), lifestyle factors (such as responses to nutrition and physical activity), and insulin pharmacology. These elements significantly affect insulin sensitivity and glycemic control in women, yet are frequently underrepresented or ignored in both research and clinical practice.
Incorporating sex-specific factors in diabetes research and treatment is essential for advancing precision medicine. There are critical gaps in understanding and applying sex-related differences. Female-specific diabetes pathophysiology manifests in three major areas: life cycle phases (including puberty, pregnancy, and menopause), lifestyle factors (such as responses to nutrition and physical activity), and insulin pharmacology. These elements significantly affect insulin sensitivity and glycemic control in women, yet are frequently underrepresented or ignored in both research and clinical practice.
Managing diabetes in women must take into account physiologic factors that are unique to females and not present in males. These sex differences are often overlooked, either due to a lack of data or a lack of appreciation for existing data. Sex is a biological feature, whereas gender encompasses the social features associated with sex.
This article focuses on sex features. Female physiology must be accounted for in three situations, including during (1) states and hormonal transitions related to the lifecycle, including the reproductive phase, pregnancy, gender-affirming hormone therapy, endocrine disorders, puberty, and menopause, (2) lifestyle management related to responses to nutrition and exercise, and (3) insulin pharmacology. Current treatment approaches for women with diabetes often fail to address critical factors related to reproductive state, life stage, and lifestyle that can all be affected by the person’s sex.
Read the study: One Size Does Not Fit All: The Need for Sex-Specific Precision Medicine in Diabetes Technology
Join Trial Testing New Oral Medication for Type 1 Diabetes by April Hopcroft for diaTribe.org, 27 May 2025.
Clinical Trials Identifier: NCT06334133
- Trial status: Recruiting
- Trial Name: Cadisegliatin as Adjunctive Therapy to Insulin in Participants With Type 1 Diabetes (CATT1)
- Diabetes Type: Type 1 diabetes
- Trial Sponsor: vTv Therapeutics
This study is testing whether the oral medication cadisegliatin can help reduce hypoglycemia in people with type 1 diabetes.
Cadisegliatin is a medication categorized as a liver-selective glucokinase activator. It is intended to help improve liver function when glucose levels are high. Specifically, cadisegliatin is believed to trap glucose within liver cells, thereby promoting glucose uptake and storage. Because cadisegliatin works differently than other diabetes medications, it may be helpful as a non-insulin medication that can be used alongside insulin to help manage blood sugar. There is currently only one such therapy approved for type 1 diabetes: Symlin (pramlintide), an injectable medication that must be taken before each meal. You may be eligible if you:
-
-
- Are 18 years or older and have been diagnosed with type 1 diabetes for at least five years
- Have an A1C under 9.5%
- Have experienced at least one hypoglycemic event with glucose below 54 mg/dL or a severe hypoglycemic event in the past two months
- Are you currently using an insulin pump or multiple daily injections
- Have used a CGM for at least three months
-
People who use automated insulin delivery (AID) systems or take non-insulin diabetes medications (such as SGLT2s, DPP-4s, GLP-1s, or metformin) are not eligible for this study.
This study is recruiting in California, Colorado, Florida, Georgia, Iowa, North Carolina, Oregon, and Texas. To enroll or learn more about this study, contact Dr. Jennifer Freeman at clinicaltrials@vtvtherapeutics.com or (336) 888-0435.
Do fat cells “remember” obesity even after weight loss? by Peter Attia, Taylor Yeater, Jess Alderman & Kathryn Birkenbach for PeterAttiaMD.com, 10 May 2025.
 For anyone who has lost a significant amount of weight, keeping it off can feel even more complicated than losing it in the first place. Even with disciplined habits and strong motivation, the body often seems to push back. Why? A new study sheds light on this frustration, suggesting that fat cells might retain a molecular “memory” of obesity, long after you’ve lost weight.
For anyone who has lost a significant amount of weight, keeping it off can feel even more complicated than losing it in the first place. Even with disciplined habits and strong motivation, the body often seems to push back. Why? A new study sheds light on this frustration, suggesting that fat cells might retain a molecular “memory” of obesity, long after you’ve lost weight.
Researchers Hinte et al. explored whether obesity leaves a biological imprint, not by altering DNA itself, but through epigenetic modifications — molecular changes that affect how the genes encoded in DNA are expressed. Their findings reveal that obesity might imprint fat cells in ways that linger, even after significant weight loss.
The results were striking: the fat cells (adipocytes) of the previously obese individuals continued to behave abnormally even two years after weight loss. In both pre- and post-weight loss adipose tissue samples, pathways related to the metabolism and function of adipocytes were consistently expressed at lower levels. In contrast, those related to fibrosis and cell death were described more than in non-obese controls. In other words, certain dysregulations in gene expression associated with obesity persist even after weight loss, causing the cells to behave as if they “remember” being obese.
Adipose tissue in formerly obese individuals retains a pro-inflammatory, metabolically altered phenotype. So while the maintained features don’t fully explain why people regain weight, they could explain why previously obese individuals remain more vulnerable to metabolic diseases, even after maintaining weight loss.
Read more: Do fat cells “remember” obesity even after weight loss?
Loneliness as deadly as obesity and smoking pack a day by Julia Musto for Independent.co.uk, 26 May 2025.
 Vivek Murthy, the former U.S. Surgeon General, is warning that the negative health impacts of chronic loneliness are comparable to some of the nation’s biggest killers. “The overall mortality increase that can be related to social disconnection is comparable to the mortality impact of smoking and obesity,” he said. “That’s how powerful and how important loneliness is.”
Vivek Murthy, the former U.S. Surgeon General, is warning that the negative health impacts of chronic loneliness are comparable to some of the nation’s biggest killers. “The overall mortality increase that can be related to social disconnection is comparable to the mortality impact of smoking and obesity,” he said. “That’s how powerful and how important loneliness is.”
He cautioned that loneliness and isolation can raise people’s risk for dangerous health conditions. Murthy astonishingly said he found that chronic loneliness is equivalent to smoking 15 cigarettes a day. “Well, it turns out that our connection with one another is not just a nice thing to have; it’s biologically an imperative for us,” he said. “It’s something we need for survival, just like we need food and water.”
This applies to those living with T1D, probably a thousand-fold! What are you doing to connect???
Read more: Loneliness as deadly as obesity and smoking pack a day
TSA issues warning about smartphones, devices at the airport. Here is what to avoid by Alex Perry for the Columbus Dispatch and published by Yahoo.com, 28 May 2025.
 The TSA has warned that USB ports, commonly used to charge cellphones, laptops, and other portable devices, can pose serious risks, making sensitive information more vulnerable to hackers and scammers. Passengers are advised to be aware of the risks associated with using the airport’s public USB charging ports. The TSA warns passengers not to plug phones or devices directly into a USB port while inside an airport, due to a cyber-theft scam called “juice/port jacking.”
The TSA has warned that USB ports, commonly used to charge cellphones, laptops, and other portable devices, can pose serious risks, making sensitive information more vulnerable to hackers and scammers. Passengers are advised to be aware of the risks associated with using the airport’s public USB charging ports. The TSA warns passengers not to plug phones or devices directly into a USB port while inside an airport, due to a cyber-theft scam called “juice/port jacking.”
Using the free USB chargers can allow hackers to access your device, bank account information, and more. Bad actors can load malware onto public USB charging stations that are commonly found in airports and hotel lobbies, according to the Federal Communications Commission. “Juice jacking” can occur when malicious actors install malware into public USB ports, aiming to steal sensitive data or hijack a device. “Malware installed through a corrupted USB port can lock a device or export personal data and passwords directly to the perpetrator,” the FCC states. “Criminals can then use that information to access online accounts or sell it to other bad actors.”
Similarly, using the airport’s free Wi-Fi can carry cybersecurity risks. The TSA advises against using the airport’s free public Wi-Fi, especially for online purchases. “Do not ever enter any sensitive info while using unsecured Wi-Fi,” TSA states. Instead of using a public USB charging port, TSA says passengers should use a TSA-compliant power brick or battery pack and plug in their devices through that, with these additional tips to help prevent falling victim to “juice jacking”:
-
-
- Using AC power outlets can help you avoid any potential risks. Pack AC, car chargers, and your own USB cables with you when traveling.
- Carry an external battery.
- Consider carrying a charging-only cable, which prevents data from being sent or received while charging, from a trusted supplier.
- If you plug your device into a USB port and a prompt appears asking you to select “share data,” “trust this computer,” or “charge only,” always select “charge only.”
-
WHY IS THIS IMPORTANT FOR THOSE WHO LIVE WITH Type 1 Diabetes: Many of us use our cellphones for automated insulin delivery systems, CGM apps, and more. The last thing you need when travelling is to lose access to your necessary mobile phones!
Read more: TSA issues warning about smartphones, devices at the airport
An open-label, multiple ascending dose trial of oral insulin Tregopil in patients with type 1 diabetes shared on PubMed.NCBI.NLM.NIH.gov, 10 April 2025.
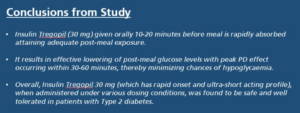 Aim: This trial evaluated the safety, tolerability, pharmacokinetics (PK) and pharmacodynamics (PD) of oral insulin Tregopil (Part 1; results discussed in this paper) and the post-prandial glucose control with different meal types in comparison with insulin aspart (Part 2) in patients with type 1 diabetes mellitus (T1DM).
Aim: This trial evaluated the safety, tolerability, pharmacokinetics (PK) and pharmacodynamics (PD) of oral insulin Tregopil (Part 1; results discussed in this paper) and the post-prandial glucose control with different meal types in comparison with insulin aspart (Part 2) in patients with type 1 diabetes mellitus (T1DM).
Results: The overall safety profile of insulin Tregopil revealed no safety concerns, except for a potential dose-dependent effect (hypoglycemia). The incidence of hypoglycaemia did not increase with increasing doses of insulin Tregopil, and none of the episodes were severe. In general, the variability of the PK/PD parameters was high. Insulin Tregopil demonstrated a rapid onset of action, with peak blood concentrations reached within 15-20 min post-dosing. Subsequently, insulin Tregopil exerted a PD effect for up to 105 min.
Conclusion: Fixed-dose insulin Tregopil reduced the requirement for insulin aspart supplementation, although it was not a viable stand-alone option for the daily management of T1DM. Insulin Tregopil could be explored with a flexible dosing approach and be titrated based on individual needs.
Trial registration: The trial is registered at Clinicaltrials.gov (CT.gov identifier: NCT04141423). The ethical approval number for the protocol is 2019146.
Read more: An open-label, multiple ascending dose trial of oral insulin Tregopil in patients with T1D
CVS, Cigna sue Arkansas to overturn new PBM law by Rebecca Pifer for HealthCareDive.com, 30 May 2025.
 CVS and Cigna have filed two separate lawsuits seeking to overturn Arkansas’s new law, which bans pharmacy benefit managers from owning or operating pharmacies in the state, from taking effect. CVS and Cigna’s PBM subsidiary, Express Scripts, filed two separate suits on Thursday in an Arkansas district court, asking a judge to declare the law unconstitutional and ban its implementation.
CVS and Cigna have filed two separate lawsuits seeking to overturn Arkansas’s new law, which bans pharmacy benefit managers from owning or operating pharmacies in the state, from taking effect. CVS and Cigna’s PBM subsidiary, Express Scripts, filed two separate suits on Thursday in an Arkansas district court, asking a judge to declare the law unconstitutional and ban its implementation.
Gov. Sarah Huckabee Sanders signed Arkansas’ legislation, called Act 624, into law in April. The law — the first of its kind — is intended to protect local community pharmacies from larger, more diversified chains by requiring companies that own both pharmacy benefit managers (PBMs) and pharmacies to close their operations in the state.
Its passage followed a groundswell of support for tackling PBM reform from lawmakers and regulators at the state and federal level, amid growing concern about rampant consolidation in the PBM industry and anticompetitive practices pursued by the most prominent players — CVS’ Caremark, Cigna’s Express Scripts and UnitedHealth’s Optum Rx, which jointly control 80% of U.S. prescriptions.
However, Arkansas’ legislation was decried by PBMs, which say it’s based on cherry-picked data and is a thinly veiled attempt to increase market share for Arkansas-owned pharmacies at the expense of out-of-state operators.
Read more: CVS, Cigna sue Arkansas to overturn new PBM law
Call Centers Replaced Many Doctors’ Receptionists. Now, AI Is Coming for Call Centers by Darius Tahir for KFFHealthNews.org, 23 May 2025.
 Startups are marketing AI-powered products with lifelike voices to schedule or cancel medical appointments, refill prescriptions, and assist with patient triage. Soon, many patients might initiate contact with the health system not by speaking with a call center worker or receptionist, but with AI. Zocdoc, the appointment-booking company, has introduced an automated assistant it says can schedule visits without human intervention 70% of the time.
Startups are marketing AI-powered products with lifelike voices to schedule or cancel medical appointments, refill prescriptions, and assist with patient triage. Soon, many patients might initiate contact with the health system not by speaking with a call center worker or receptionist, but with AI. Zocdoc, the appointment-booking company, has introduced an automated assistant it says can schedule visits without human intervention 70% of the time.
A medically focused call center workforce in the Philippines is vast, with an estimated 200,000 members by the end of 2024, according to Jack Madrid, leader of the industry trade group. That figure exceeds the number of paramedics in the United States at the end of 2023, according to the Bureau of Labor Statistics. Some employers are opening outposts in other countries, such as India, while using AI to reshape or replace their workforces.
It’s unclear whether AI’s digital manipulations could match the proverbial human touch. “The rapport, or the trust that we give, or the emotions that we have as humans cannot be replaced,” Ruth Elio, an occupational nurse who supervised the center’s workers, said. Sachin Jain, president and CEO of Scan Health Plan, an insurer, said humans have context that AI doesn’t have, at least for now. A receptionist at a small practice may know the patients well enough to pick up on subtle cues and communicate to the doctor that a particular caller is “somebody that you should see, talk to, that day, that minute, or that week.”
The turn toward call centers, while creating more distance between a caller and a health provider, preserved the human touch. Yet some agents at call centers and their advocates say the ways they are monitored on the job undermine care. At one Kaiser Permanente location, “From the beginning of the shift to your end, you’re expected to take call after call after call from an open queue,” an employee said. Even when giving advice for complex cases, “there’s an unwritten rule on how long a nurse should take per call: 12 minutes.”
Read more: Call Centers Replaced Many Doctors’ Receptionists. Now, AI Is Coming for Call Center


