Know Labs reports data from feasibility study of Bio-RFID sensor reported on MedicalDevice-Network.com, 8 May 2023.
 Know Labs has reported data from a new technical feasibility study of its Bio-RFID sensor technology for non-invasive glucose monitoring, compared to Dexcom G6 device. The results of the study were presented at the American Association of Clinical Endocrinology (AACE) Annual Meeting in Seattle, Washington.
Know Labs has reported data from a new technical feasibility study of its Bio-RFID sensor technology for non-invasive glucose monitoring, compared to Dexcom G6 device. The results of the study were presented at the American Association of Clinical Endocrinology (AACE) Annual Meeting in Seattle, Washington.
The company conducted a series of internal studies from December last year through February this year, to confirm the technical feasibility of its Bio-RFID sensor technology. The technical feasibility study was carried out to showcase the stability of the hardware and software infrastructure of the sensor. Another objective was to collect further data to validate the sensor’s accuracy in quantifying blood glucose concentration (BGC) in vivo non-invasively using radio frequency.
Know Labs chief product officer Steve Kent said: “We have successfully completed our foundational studies, we have a stable sensor that delivers repeatable results, and we have developed software infrastructure to manage and interpret large, novel datasets.
Read more: Know Labs reports data from feasibility study of Bio-RFID sensor
Time in range similar with fast-acting vs. standard insulin for young kids with diabetes by Michael Monostra for Healio.com/endocrinology, 8 May 2023.
 Fast-acting insulin aspart delivered through a hybrid closed-loop insulin delivery system provided similar glycemic outcomes as standard insulin aspart for young children with type 1 diabetes, according to study data. The study cohort had a baseline HbA1c of 7.2% and a time in range of 63.9% at the start of the trial. Of the cohort, 76% was using a hybrid closed-loop insulin delivery system at enrollment.
Fast-acting insulin aspart delivered through a hybrid closed-loop insulin delivery system provided similar glycemic outcomes as standard insulin aspart for young children with type 1 diabetes, according to study data. The study cohort had a baseline HbA1c of 7.2% and a time in range of 63.9% at the start of the trial. Of the cohort, 76% was using a hybrid closed-loop insulin delivery system at enrollment.
Time in range was similar between fast-acting insulin aspart and standard insulin aspart. No differences were seen for time spent in hypoglycemia, time spent in hyperglycemia or glucose variability. Children received slightly more insulin when using fast-acting insulin aspart compared with standard insulin aspart (0.74 U/kg per day vs. 0.72 U/kg per day; P = .04). The higher daily insulin total with fast-acting insulin aspart was due to a higher basal insulin delivery. Closed-loop usage was similar between both therapies, and sensor glucose metrics were similar during both daytime and nighttime.
Hyperglycemia with ketosis more common with fast-acting insulin: There was no difference in the levels of diabetes distress or hypoglycemia fear between the two interventions, though researchers noted a trend toward less hypoglycemia worry with fast-acting insulin aspart.
Read more: Time in range similar with fast-acting vs. standard insulin for young kids with diabetes
Insulin Resistance and Type 1 Diabetes by Marissa Town for ChildrenWithDiabetes.com, 4 May 2023.
 Insulin resistance is when the cells in the body have a reduced response to insulin and is considered the hallmark in diagnosing type 2 diabetes. It has been shown in recent research that people with type 1 diabetes develop insulin resistance over time, possibly related to the use of what is called exogenous insulin (insulin that comes from outside the body). We also know that many people have what has been termed “double diabetes,” where the individual has both insulin resistance and a lack of the ability to make insulin.
Insulin resistance is when the cells in the body have a reduced response to insulin and is considered the hallmark in diagnosing type 2 diabetes. It has been shown in recent research that people with type 1 diabetes develop insulin resistance over time, possibly related to the use of what is called exogenous insulin (insulin that comes from outside the body). We also know that many people have what has been termed “double diabetes,” where the individual has both insulin resistance and a lack of the ability to make insulin.
There are some times in life where insulin resistance is normal such as puberty, pregnancy, and during use of steroids. Luckily, these are all temporary and when the hormones or steroids are out of the system, insulin resistance should go back to normal. For people with diabetes using insulin therapy, there is unfortunately no end in sight for the need of insulin use, and newer studies suggest that using insulin that is not endogenous (made by your own body) causes insulin resistance.
For those of us who require exogenous insulin to live, extra insulin collects in our body which causes the cells to adapt and reduce the number of receptors for insulin. This in turn increases the amount of insulin needed, which can further lead to having excess insulin and further reduction in receptors. Other causes of increased insulin resistance include weight gain, physical inactivity, high triglycerides, defects on the insulin receptors of cells, stress on the body, chronic inflammation, and genetic predisposition, among others.
Measuring insulin sensitivity or resistance used to involve “euglycemic clamp” studies in which people are put on IV’s and insulin and glucose are infused to keep the blood glucose at a normal level. This is very costly, invasive, and time consuming. Unfortunately, you cannot determine insulin resistance based on how much insulin someone with type 1 diabetes is taking compared to their body weight.
Read more: Insulin Resistance and Type 1 Diabetes
New capsule dives deep into your digestive system to study microorganisms by Sejal Sharma for InterestingEngineering.com, 11 May 2023.
 The human intestinal tract is home to a vast majority of microorganisms residing in our bodies. Humans depend on these microorganisms for food digestion, protection against pathogens, and immune system regulation, among other critical functions. How these microorganisms interact in the gut is usually studied by assessing the human stool due to difficulties in sampling the intestinal tract.
The human intestinal tract is home to a vast majority of microorganisms residing in our bodies. Humans depend on these microorganisms for food digestion, protection against pathogens, and immune system regulation, among other critical functions. How these microorganisms interact in the gut is usually studied by assessing the human stool due to difficulties in sampling the intestinal tract.
Making a significant pathway in furthering human gut microbiome studies, a group of researchers at UC Davis have developed a capsule that can literally deep dive into our digestive system and collect important information about micro inhabitants and our digestion process. Researchers explain in a statement that their new capsule, called CapScan, is administered orally.
The researchers then analyzed contents like bacteria, viruses, host proteins, and metabolism in the upper intestine. They found that these contents in the upper intestine and stool differed dramatically in all 15 study individuals. The team also factored in their diet, alcohol intake, fruit consumption, and metabolism. Additionally, it was found that two subjects who had taken antibiotics six months before the study had different variations of bioactive fatty acid esters of hydroxy fatty acids, or FAFHAs, and sulfonolipids, metabolites which are associated with preventing diabetes and inflammation, said the statement. “Overall, this device can help elucidate the roles of the gut microbiome and metabolome in human physiology and disease,” added Fiehn. The study was published in the journal Nature.
Read more: New capsule dives deep into your digestive system to study microorganisms
Insulin thermostability in a real-world setting was published in TheLancet.com/Diabetes & Endocrinology, 29 March 2023.
 Various forms of diabetes care necessitate exogenous insulin replacement. Administered insulin must have predictable potency to avoid potentially dangerous glycaemic excursions. However, insulin is temperature sensitive, with potency reduced through rising temperatures. Insulin manufacturers and regulatory agencies direct that insulin be refrigerated (at 4–6°C), never frozen, and with a maximum usage or storage period of approximately 1 month at standard room temperatures (20–25°C).
Various forms of diabetes care necessitate exogenous insulin replacement. Administered insulin must have predictable potency to avoid potentially dangerous glycaemic excursions. However, insulin is temperature sensitive, with potency reduced through rising temperatures. Insulin manufacturers and regulatory agencies direct that insulin be refrigerated (at 4–6°C), never frozen, and with a maximum usage or storage period of approximately 1 month at standard room temperatures (20–25°C).
This requirement is especially challenging in hot climate settings if home refrigeration is unavailable, which is the case for some 770 million people. Furthermore, in some situations, insulin must also be stored for a few months due to clinic visit frequency, travel costs, and intermittent pharmacy supplies. In response to this, many families use evaporative cooling with clay pots to assist in reducing insulin storage temperatures, by storing insulin within an air-filled space or a sealed bag in clay pots.
Data regarding insulin stability outside the recommendations are scarce. In 1968, Storvick and Henry reported that animal-derived isophane insulin retained 95% or more of its potency for 12 months at 25°C. In 1972, Pingel and Volund found that similar isophane and soluble insulins retained 95% or more of their potency for at least 5 months at temperatures of up to 30°C. A study using human insulin showed loss of some potency during storage at 32–37°C for 28 days, whereas a recent study showed that the potency of human and analog insulin remained unchanged at oscillating temperatures of 25–37°C for 28 days and 12 weeks.
This study of insulin thermostability outside refrigeration, during the summer in India, showed that acceptable insulin concentrations were maintained for up to 2 months for all samples of all insulin preparations. At 4 months, all samples from three analog insulin preparations and three of four samples for each of the human insulins also maintained a relative concentration of 95% or more.
Read more: Insulin thermostability in a real-world setting
Watermelons may improve diet quality and cardiometabolic health by Annie Lennon for MedicalNewsToday.com, 10 May 2023.
 Watermelons contain many nutrients, such as potassium, vitamin C, and magnesium. The fruit also has a high bioavailability of antioxidants, including lycopene and l-citrulline. Studies have shown that watermelon supplements and extracts decrease blood pressure and cholesterol levels. Comparably fewer studies investigate raw watermelon, however, and those that do tend to involve large quantities of over 2 lbs per day. Nevertheless, these studies also report that consumption of the fruit is linked to lower cholesterol and body weight, as well as a lower risk of prostate, lung, and breast cancer.
Watermelons contain many nutrients, such as potassium, vitamin C, and magnesium. The fruit also has a high bioavailability of antioxidants, including lycopene and l-citrulline. Studies have shown that watermelon supplements and extracts decrease blood pressure and cholesterol levels. Comparably fewer studies investigate raw watermelon, however, and those that do tend to involve large quantities of over 2 lbs per day. Nevertheless, these studies also report that consumption of the fruit is linked to lower cholesterol and body weight, as well as a lower risk of prostate, lung, and breast cancer.
Recently, two studies that investigated the health effects of watermelon consumption. The first study, published in Nutrients, found that children and adults who consumed watermelon had a higher intake of various nutrients, including dietary fiber, magnesium, and potassium, than non-consumers. They also had a lower intake of added sugars and saturated fatty acids. The second study, also published in Nutrients, found that drinking watermelon juice for two weeks protects vascular function.
Dr. Rigved Tadwalkar, a board-certified cardiologist at Providence Saint John’s Health Center in Santa Monica, California, who was not involved in these studies, said that some may not consider watermelon as part of a heart-healthy diet due to its high sugar content. He noted, however, that the sugars in the fruit have a low glycemic index meaning they impact blood sugar less than sugars from other sources. He added that the fruit’s high fiber and water content may also mitigate the effects on blood sugar when consumed moderately.
Read more: Watermelons may improve diet quality and cardiometabolic health
Embecta and Tidepool partner to develop automated insulin delivery system for people with Type 2 diabetes by Embecta Corp. reported on GlobeNewsWire.com, 12 May 2023.
 Embecta Corp. (“embecta”), one of the largest pure-play diabetes care companies in the world, and Tidepool, a 501(c)(3) nonprofit organization committed to harnessing the power of technology to provide intuitive software products that help people living with diabetes, have announced that the two organizations will partner to develop an automated insulin delivery (AID) system for people living with type 2 diabetes (T2D). embecta will leverage Tidepool’s expertise in diabetes management software to develop the AID algorithm for its closed-loop patch pump system designed with the specific needs of people living with T2D, for which it received FDA Breakthrough Device Designation.
Embecta Corp. (“embecta”), one of the largest pure-play diabetes care companies in the world, and Tidepool, a 501(c)(3) nonprofit organization committed to harnessing the power of technology to provide intuitive software products that help people living with diabetes, have announced that the two organizations will partner to develop an automated insulin delivery (AID) system for people living with type 2 diabetes (T2D). embecta will leverage Tidepool’s expertise in diabetes management software to develop the AID algorithm for its closed-loop patch pump system designed with the specific needs of people living with T2D, for which it received FDA Breakthrough Device Designation.
“A large segment of the diabetes community is made up of people living with T2D, however, the existing AID systems are not tailored to meet their unique needs,” said Henry Anhalt, DO, Chief Medical Officer, embecta. “The recent 510(k) clearance of Tidepool Loop — a fully interoperable automated insulin dosing app which started as a patient-led initiative — affirms that Tidepool’s approach to AID system development combines patient insights with a robust diabetes management solution. We believe that the combination of the embecta and Tidepool teams will lead to the development of a user-centric T2D AID system that fills a need for improved glucose management.”
Read more:
Glucomate: A New iPhone App for Analyzing Your Glucose Data by Arvind Sommi for diaTribe.org, 8 May 2023.
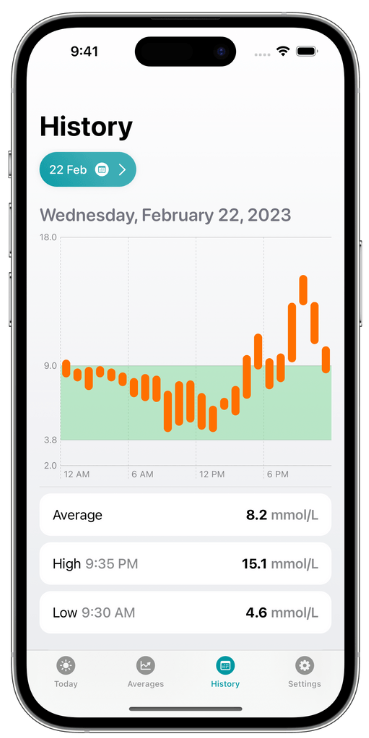 Glucomate is a new iPhone app that helps people manage their diabetes. The developer found it challenging to make use of all the data that was collected from his continuous glucose monitor, so he decided to create an app that could help him and others in a similar situation.
Glucomate is a new iPhone app that helps people manage their diabetes. The developer found it challenging to make use of all the data that was collected from his continuous glucose monitor, so he decided to create an app that could help him and others in a similar situation.
Users can view specific dates to see what data was collected on that day, identify trends, and see glucose levels during specific activities. For example, if you have an Apple Watch and track your workouts, Glucomate can help you identify the effect that certain exercises have on your blood glucose levels. The app also lets users manually add data from your iPhone or Apple Watch. Historical data can display averages, high/low information, time in range, as well as charts based on 7, 14, 30, or 90 days of readings. This feature can help users spot trends and make better decisions on how to manage their glucose levels.
While some of these features are free, the full version of Glucomate can be purchased for $1.99 per month, $14.99 per year, or as a one-time $59.99 lifetime unlock.
The developer, Zach Simone, has been building apps for the iPhone for almost 10 years, and has always been passionate about building good-looking apps that are easy to use and solve a need for the people using them. He’s also had type-1 diabetes for over 20 years, and has an interest (totally not an obsession…) in knowing what his glucose levels are doing. The idea for Glucomate came almost 6 years ago when he started using a continuous glucose monitor (CGM) which records glucose levels every 5 minutes.
Read more: Glucomate: A New iPhone App for Analyzing Your Glucose Data
Diabetes is now an epidemic in the UK by Jason Goodyer for ScienceFocus.com, 10 May 2023.
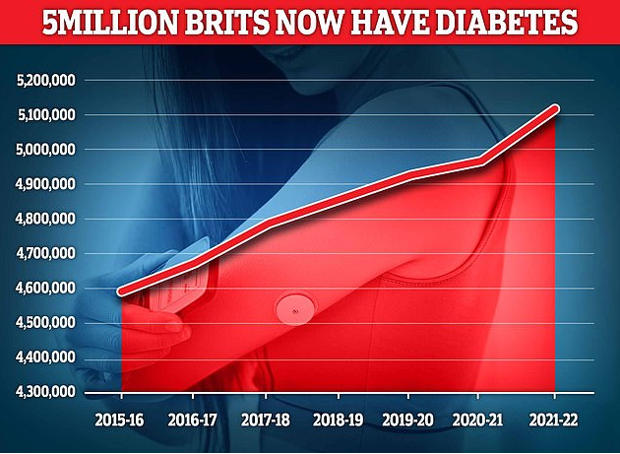 A recent report carried out by Diabetes UK has found that the number of people living with diabetes in the UK has topped 5 million for the first time ever. This includes an estimated of 850,000 people that are as yet undiagnosed based on Association of Public Health Observatories projections.
A recent report carried out by Diabetes UK has found that the number of people living with diabetes in the UK has topped 5 million for the first time ever. This includes an estimated of 850,000 people that are as yet undiagnosed based on Association of Public Health Observatories projections.
for the first time there are over 5 million people living with diabetes in the UK. The split is about roughly 90 per cent type 2 diabetes, 8 per cent type 1 diabetes and 2 per cent other types of diabetes.
Read more: Diabetes is now an epidemic in the UK
Bills in 30 states show momentum to fix prior authorization by Kevin B. O’Reilly for AMA-Assn.org, 10 May 2023.
 A majority of U.S. states are considering legislation to rightsize the time-wasting, care-delaying payer practice of prior authorization. In all, nearly 90 prior-authorization reform bills have been considered this legislative session in 30 states, and more than a dozen are still on the table for potential passage.
A majority of U.S. states are considering legislation to rightsize the time-wasting, care-delaying payer practice of prior authorization. In all, nearly 90 prior-authorization reform bills have been considered this legislative session in 30 states, and more than a dozen are still on the table for potential passage.
Many of the bills draw on the AMA’s model legislation (PDF) and encompass prior-authorization reforms to:
-
-
- Establish quick response times (24 hours for urgent, 48 hours for nonurgent care).
- Allow adverse determinations only by a physician licensed in the state and of the same specialty that typically manages the patient’s condition.
- Prohibit retroactive denials if care is preauthorized.
- Make authorization valid for at least one year, regardless of dose changes; and for those with chronic conditions, the prior authorization should be valid for the length of treatment.
- Require public release of insurers’ prior authorization data by drug and service as it relates to approvals, denials, appeals, wait times and more.
- Require a new health plan to honor the patient’s prior authorization for at least 90 days.
- Reduce volume through the use of solutions such as prior authorization exemptions or gold-carding programs.
-
“The momentum behind prior-authorization reform feels powerful right now, with dozens of bills in state legislatures this year and advocates laying the groundwork for next year,” said AMA President Jack Resneck Jr., MD.


Oh, I love Watermelon. I mean I love it. Man, does it ever mess with my blood sugar. But I did love it. I think the gut bacteria capsule is such a good idea.
The reason for the same TIR in both the fast acting and regular acting insulin is the spread of TIR. The key I think would be tighten TIR parameters to 90 to 140. If the fastest acting insulin can cut the upside number to perhaps 140 then the cost would be 100% worth it. But it will never pay to use the higher cost insulin on the same old scale.
Thankfully, I seem to do ok with watermelon!