Diabeloop’s Automated Tech Aims at ‘Zen’ for Diabetes Control was written by Mike Hoskins for DiabetesMine.com, 3 March 2021. I WANT THIS!!!
 French company Diabeloop stands out for its design work. This is because the company works on their designs with input from the people who will actually be using their products. Company leaders have worked directly with people with diabetes in the DIY #WeAreNotWaiting community to create a more customizable, practical system instead of the usual “engineering-driven” devices.
French company Diabeloop stands out for its design work. This is because the company works on their designs with input from the people who will actually be using their products. Company leaders have worked directly with people with diabetes in the DIY #WeAreNotWaiting community to create a more customizable, practical system instead of the usual “engineering-driven” devices.
Diabeloop “Zen Mode” feature lets users temporarily raise glucose targets slightly to avoid annoying alerts that would otherwise beep after every meal. There’s also a “Privacy Mode” that lets them shut off sharing features in case they need a break. While it hasn’t yet hit the market, Diabeloop expects to launch its first-generation system in Europe during 2021. From there, the plan is for a U.S. launch before long.
 Diabeloop’s key technology is a smart algorithm that functions as the brains of its new automated insulin delivery system, preliminarily known as DBLG1 (for “Generation 1,” to be followed by DBLG2). Unlike the two commercial systems currently on the market in the U.S. from Medtronic and Tandem, this Diabeloop smart algorithm works on a dedicated handheld receiver or smartphone app. It then communicates with a connected insulin pump and continuous glucose monitor (CGM). Diabeloop’s artificial intelligence (AI) analyzes glucose data, calculates insulin amounts, and automates the pump delivery based on the CGM readings.
Diabeloop’s key technology is a smart algorithm that functions as the brains of its new automated insulin delivery system, preliminarily known as DBLG1 (for “Generation 1,” to be followed by DBLG2). Unlike the two commercial systems currently on the market in the U.S. from Medtronic and Tandem, this Diabeloop smart algorithm works on a dedicated handheld receiver or smartphone app. It then communicates with a connected insulin pump and continuous glucose monitor (CGM). Diabeloop’s artificial intelligence (AI) analyzes glucose data, calculates insulin amounts, and automates the pump delivery based on the CGM readings.
Diabeloop’s first generation works with the colorful hybrid patch-tubed Kaleido pump available outside the U.S., but the company hopes to work with other in-development devices down the road.
Read more: Diabeloop’s Automated Tech Aims at ‘Zen’ for Diabetes Control
Lilly and Biolojic Design Announce Research Collaboration to Discover and Develop Antibody Therapies for Diabetes was reported on SeekingAlpha.com, 8 March 2021.
 Eli Lilly and Company and Biolojic Design Ltd., a biotechnology company that computationally designs functional antibodies, today announced a research collaboration and license agreement that will leverage Biolojic’s AI-based multibody platform to discover and develop a potential novel antibody-based therapy for the treatment of diabetes.
Eli Lilly and Company and Biolojic Design Ltd., a biotechnology company that computationally designs functional antibodies, today announced a research collaboration and license agreement that will leverage Biolojic’s AI-based multibody platform to discover and develop a potential novel antibody-based therapy for the treatment of diabetes.
A multi-specific antibody, or multibody, is a human antibody that is computationally engineered to bind two or more targets at each of its arms. Fine-tuning the affinity and respective competition of the two targets can produce therapies with differential activities, which vary depending on tissue localization and metabolic parameters. The specific targets to be studied in the collaboration were not disclosed.
 Biolojic Design is committed to curing patients by designing and developing a pipeline of revolutionary therapeutics. Powered by AI, Biolojic’s technology designs single and multi-specific antibodies precisely targeting predefined epitopes to execute novel biological programs. Focusing on diseases that involve the immune system, Biolojic develops a pipeline of antibodies that are designed to unlock the full potential of well-studied pathways.
Biolojic Design is committed to curing patients by designing and developing a pipeline of revolutionary therapeutics. Powered by AI, Biolojic’s technology designs single and multi-specific antibodies precisely targeting predefined epitopes to execute novel biological programs. Focusing on diseases that involve the immune system, Biolojic develops a pipeline of antibodies that are designed to unlock the full potential of well-studied pathways.
Read more: Lilly and Biolojic Design Announce Research Collaboration to Discover and Develop Antibody Therapies
Experimental Drug May Fight Type 1 Diabetes was reported by Amy Norton for WebMD.com, 8 March 2021. Just two weeks of treatment with an experimental drug can delay the onset of type 1 diabetes by several years, researchers report.
 The drug, called teplizumab, is already under review by the U.S. Food and Drug Administration based on earlier evidence of its effectiveness. If it gets the green light, it would become the first drug approved for delaying type 1 diabetes in high-risk people. In this latest follow-up, the investigators found that half of patients given teplizumab were still diabetes-free five years later, versus only 22% of the placebo group.
The drug, called teplizumab, is already under review by the U.S. Food and Drug Administration based on earlier evidence of its effectiveness. If it gets the green light, it would become the first drug approved for delaying type 1 diabetes in high-risk people. In this latest follow-up, the investigators found that half of patients given teplizumab were still diabetes-free five years later, versus only 22% of the placebo group.
The teplizumab trial was sponsored by the Type 1 Diabetes TrialNet Study Group, a network funded by the U.S. National Institutes of Health and JDRF. The drug, being developed by the biotech company Provention, was awarded “breakthrough” status by the FDA, which means it will get an expedited review. An approval could come as early as this summer, according to Dr. Kevan Herold, a professor at Yale University who led the trial.
Read more: Experimental Drug May Fight Type 1 Diabetes
Could transforming alpha cells into beta cells treat diabetes? was written by James Kingsland for MedicalNewsToday.com, 4 March 2021.
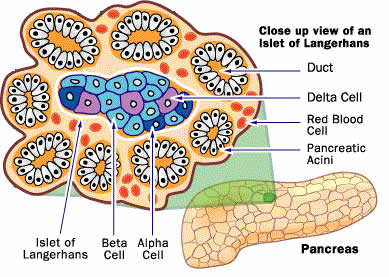 Scientists have used synthetic antibodies to block cell receptors in the liver that normally bind to glucagon, a hormone involved in increasing the amount of glucose in the blood. The antibodies restored normal blood glucose levels in three different mouse models of diabetes. The treatment partly worked by transforming alpha cells in the pancreas into insulin-producing beta cells. The researchers believe that the same approach could treat type 1 and type 2 diabetes in people.
Scientists have used synthetic antibodies to block cell receptors in the liver that normally bind to glucagon, a hormone involved in increasing the amount of glucose in the blood. The antibodies restored normal blood glucose levels in three different mouse models of diabetes. The treatment partly worked by transforming alpha cells in the pancreas into insulin-producing beta cells. The researchers believe that the same approach could treat type 1 and type 2 diabetes in people.
In healthy individuals, the concentration of glucose in the blood is maintained at optimum levels through the opposing effects of two hormones, insulin and glucagon. Beta cells in the pancreas produce insulin, which stimulates cells around the body to extract glucose from the bloodstream. Other cells in the pancreas, called alpha cells, produce glucagon, which increases the amount of glucose that the liver releases into the bloodstream.
A team led by researchers at the University of Texas Southwestern Medical Center, in Dallas, has discovered that blocking glucagon receptors has the indirect effect of transforming alpha cells in the pancreas into beta cells. The newly created beta cells produce insulin, which helps lower levels of glucose circulating in the blood.
Though people with type 1 or type 2 diabetes “try their very best to keep glucose under control, it fluctuates quite massively throughout the day, even with the best state-of-the-art pump,” explains study leader Dr. May-Yun Wang, an assistant professor of internal medicine at the medical center.
“Giving them back their own beta cells could help restore much better natural regulation, greatly improving glucose regulation and quality of life,” she continues. Transforming alpha cells into beta cells could be a particularly promising treatment for type 1 diabetes, says Dr. William L. Holland, the senior study author, who is now an assistant professor of nutrition and integrative physiology at the University of Utah, in Salt Lake City.
Read more: Could transforming alpha cells into beta cells treat diabetes?


But if my Alpha became my Beta, could I still be an A-Z person? Or, would my High School English teacher be right? Would I really be missing a few pieces somewhere?
LOL
Don’t worry I know he she was right.