Meet HARPA, the bold way Biden can jump-start health innovation was published by Ruth Reader for FastCompany.com, 12 February 2021. The Biden administration is contemplating creating a research agency to help fund breakthroughs that aren’t economically viable for big health and pharmaceutical companies. Meet HARPA.
 As part of his first-100-days effort, President Biden’s administration is working to form a new agency that could change the face of healthcare: an Advanced Research Projects Agency for Health. This new agency would pay academics and private companies to develop innovative health products and services, mimicking the process of the Defense Advanced Research Projects Agency (DARPA), whose work helped create the internet. The goal would be to create a government engine that could help advance innovation into real-world products for healthcare that could solve persistent problems: high drug costs, lack of treatments for rare diseases, poor systems of care, and of course, pandemic preparedness.
As part of his first-100-days effort, President Biden’s administration is working to form a new agency that could change the face of healthcare: an Advanced Research Projects Agency for Health. This new agency would pay academics and private companies to develop innovative health products and services, mimicking the process of the Defense Advanced Research Projects Agency (DARPA), whose work helped create the internet. The goal would be to create a government engine that could help advance innovation into real-world products for healthcare that could solve persistent problems: high drug costs, lack of treatments for rare diseases, poor systems of care, and of course, pandemic preparedness.
“Innovations in biomedical research are right now largely funded by the private sector or through organizations like the [National Institutes of Health],” says Mike Stebbins, a geneticist and former assistant director for biotechnology at the White House Office of Science and Technology Policy, who has been campaigning for the formation of HARPA for years. “The problem is you’ve only got a $40 billion budget for the NIH annually, and they fund very little in the way of research on products.”
Read more: Meet HARPA, bold way to jump-start health innovation
Self-Healing Wearable Turns Your Body Into a Battery was reported by Loukia Papadopoulos for InterestingEngineering.com, 13 February 2021. The device uses thermoelectric generators to convert the body’s internal temperature into electricity.
 It’s the stuff of science fiction: using your own body to power your electronics. And yet it is finally here. Does this mean we won’t have to constantly charge our devices or carry batteries???
It’s the stuff of science fiction: using your own body to power your electronics. And yet it is finally here. Does this mean we won’t have to constantly charge our devices or carry batteries???
Researchers at CU Boulder have developed a new, low-cost wearable device that is stretchy enough that you can wear it like a ring, a bracelet, or any other accessory and it transforms the human body into a battery.
“In the future, we want to be able to power your wearable electronics without having to include a battery,” said in a statement Jianliang Xiao, senior author of the new paper and an associate professor in the Paul M. Rady Department of Mechanical Engineering at CU Boulder.
His new devices can generate about one volt of energy for every 0.155 sq in (1 sq cm) of skin space, enough to power electronics such as watches. The wearables tap into a person’s natural body heat, using thermoelectric generators to convert the body’s internal temperature into electricity. Even better, the device can heal itself when damaged and is fully recyclable.
Read more: Self-Healing Wearable Turns Your Body Into a Battery
What is C-Peptide? was posted on ChildrenwithDiabetes.com, 10 February 2021.
 C-peptide is a measure of how the beta cells in the pancreas are making insulin. It is a hormone produced by the pancreas, released at the same time as insulin. It has no effect on blood sugar but is a useful marker of insulin production, since the pancreas usually releases c-peptide and insulin in equal amounts. You may have had it measured at diagnosis or in preparation for getting an insulin pump because your insurance required it. Odds are if you have had type 1 for a while your levels will be close to 0. But if you have recently been diagnosed or have type 2, you may have higher levels of c-peptide and insulin production.
C-peptide is a measure of how the beta cells in the pancreas are making insulin. It is a hormone produced by the pancreas, released at the same time as insulin. It has no effect on blood sugar but is a useful marker of insulin production, since the pancreas usually releases c-peptide and insulin in equal amounts. You may have had it measured at diagnosis or in preparation for getting an insulin pump because your insurance required it. Odds are if you have had type 1 for a while your levels will be close to 0. But if you have recently been diagnosed or have type 2, you may have higher levels of c-peptide and insulin production.
Why does it even matter? It happens often, but a misdiagnosis can cause challenges in achieving blood glucose and A1C goals. In particular, Maturity-Onset Diabetes of the Young (MODY) is typically misdiagnosed as type 1 and c-peptide can help detect MODY before pursuing further genetic testing. It can also show whether or not someone with type 2 diabetes may require insulin.
Higher levels of c-peptide have been shown to be protective of diabetes complications in various studies including the pivotal the Diabetes Complications and Control Trial (DCCT). Additionally, people with lower levels of c-peptide have a greater risk of glucose variability and severe low blood sugars. Another study on 6,076 people with diabetes in Scotland showed that even small amounts of residual c-peptide could help reduce complications including DKA, retinopathy, and severe hypoglycemia.
It also has been shown that people who are diagnosed at younger ages are more likely to have a lower c-peptide level and those diagnosed over the age of 18 are more likely to have some residual c-peptide and insulin production. It is important to note that this does not mean you won’t need insulin if your c-peptide is detectable.
Read more: What is C-Peptide?
Now let’s take a look at Diabetic Neuropathic Pain:
Targeting the Proopiomelanocortin Pathway for Diabetic Neuropathic Pain was written by Laren Biscaldi for EndocrinologyAdvisor.com, 2 February 2021.
 Reinstating the proopiomelanocortin (POMC) pathway can overcome neuropathic pain, representing a potential therapeutic target for future diabetic neuropathic pain therapies, according to research published in Nature Communications.
Reinstating the proopiomelanocortin (POMC) pathway can overcome neuropathic pain, representing a potential therapeutic target for future diabetic neuropathic pain therapies, according to research published in Nature Communications.
Sensorimotor neuropathy is common in diabetes, with about half of individuals with diabetic peripheral neuropathy (DPN) presenting with chronic symptoms of neuropathic pain. Current treatment approaches include drugs serotonin-norepinephrine reuptake inhibitors, sodium channel blockers, opioids, and tight blood glucose control. An improved analgesic treatment is desirable to improve on the current generalized therapies available, according to researchers.
“Our study demonstrates the presence of the endogenous opioid precursor, POMC, in the sensory ganglia of mice and humans and its importance in antinociception, especially during painful DPN,” the researchers wrote, adding that during diabetes, the POMC µ-opioid receptor (MOR) opioid pathway becomes “dysfunctional” at both the ligand and receptor level. These findings explain why MOR-targeting opioids, such as tramadol and oxycodone, do not uniformly provide relief in people with DPN.
Read more: Proopiomelanocortin Pathway for Diabetic Neuropathic Pain
Capsaicin 8% Safe and Effective for Diabetic Peripheral Nerve Pain Therapy was reported by Lauren Biscaldi for EndocrinologyAdvisor.com, 29 January 2021.
 A high-concentration capsaicin 8% patch is both effective and well-tolerated as a treatment option for diabetic peripheral nerve pain (DPNP), either alone or in combination with standard oral therapies, according to a review published in the Expert Review of Neurotherapeutics.
A high-concentration capsaicin 8% patch is both effective and well-tolerated as a treatment option for diabetic peripheral nerve pain (DPNP), either alone or in combination with standard oral therapies, according to a review published in the Expert Review of Neurotherapeutics.
Approximately half of all adults with diabetes experience diabetic peripheral neuropathy; about 25% of these adults experience DPNP that severely affects quality of life and is a significant cause of morbidity.
At this time, there is no approved treatment that can reverse or prevent DPN disease progression. Current pharmacologic management of DPN pain focuses on glycemic control and symptomatic therapies and includes α-2-δ ligands, tricyclic antidepressants, and serotonin-norepinephrine reuptake inhibitors.
Topical treatment modalities for DPNP include low-dose capsaicin creams (0.025%-0.075%). These creams have demonstrated moderate efficacy but are often poorly tolerated because of frequent reapplication needs and burning sensation at the application site.
Read more: Capsaicin 8% Safe, Effective for Diabetic Peripheral Nerve Pain Therapy
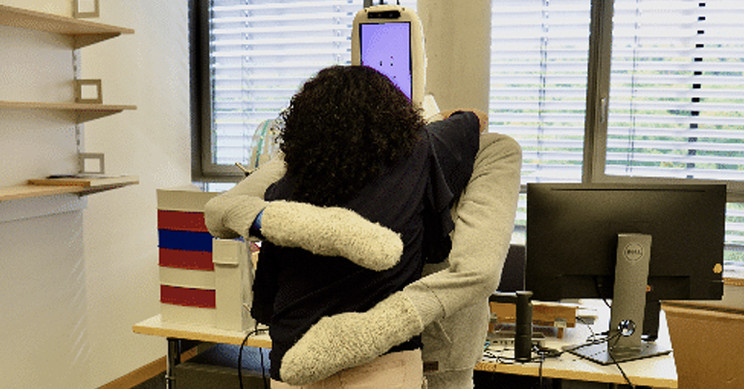
Soft, Human-Sized Robot Gives Excellent Hugs is written by Derya Ozdemir for InterestingEngineering.com, 12 February 2021. Once you get over the awkwardness, receiving a hug from a robot could be as good as the real thing.
 There’s a reason why we get the urge to squeeze someone lovingly from time to time, and like most things are, it’s got to do with health. From lowering blood pressure and cortisol levels to alleviating stress and anxiety, a hug a day keeps a good job of keeping the doctor away; however, amid a time a casual hug between acquaintances seems so far away, science had got to get creative.
There’s a reason why we get the urge to squeeze someone lovingly from time to time, and like most things are, it’s got to do with health. From lowering blood pressure and cortisol levels to alleviating stress and anxiety, a hug a day keeps a good job of keeping the doctor away; however, amid a time a casual hug between acquaintances seems so far away, science had got to get creative.
A team of researchers at the Max Planck Institute for Intelligent Systems (MPI-IS) and ETH Zürich have recently come up with a HuggieBot 2.0 that can deliver a loving embrace when requested.
HuggieBot 2.0 builds on a previous system created by Alexis E. Block, one of the authors, who come up with it after being inspired by her family members who were far away whom she wanted to give a big hug. HuggieBot 1.0, based on a robotic platform created by Willow Garage, was apparently too bulky to be a good hugger, and it couldn’t feel the user well because it had only one touch sensor located on its back.
“Our new robotic platform was built according to our six design tenets, or ‘commandments’ for natural and enjoyable robotic hugging,” Block said to Tech Explore. “Namely, we felt that a hugging robot should be soft, be warm, be human-sized, visually perceive its user, adjust its embrace to the user’s size and position and reliably release when the user wants to end the hug. By following these commandments, HuggieBot 2.0 gives excellent hugs.”
The HuggieBot 2.0 and HuggieBot 3.0 are still prototypes, but one day, the researchers want to commercialize the concept. The researchers are also developing HuggieApp which will allow users to remotely send each other customized hugs via the HuggieBot robot.
This robot will be presented at the ACM/IEEE International Conference on Human-Robot Interaction (HRI) in March.
Read more: Soft, Human-Sized Robot Gives Excellent Hugs


I know my mom used lots of capsaicin for Diabetic Neuropathic Pain yet it never helped. I hope it helps many. In fact the other article about neuropathy gives me great hope that it might work. The pain is so difficult I so hope an answer can be found.
By the way I do not think even the huggy bot would help that much. 🙂