In this week’s issue of The Savvy Diabetic:
- Sequel Twiist/Eversense CGM
- Adocia AdoShell Immunoprotective Hydrogel for Islets
- How To Treat a HYPO
- Zucara Therapeutics ZT-01 Once-Daily to Prevent Hypoglycemia
- GLP-1s – One Class of Drugs with Many Different Names
- Mounjaro vs Ozempic
- Semaglutide effectively treats liver disease in two-thirds of patients
- GLP-1s Could Help People Sleep Better
- This Is Your Body on Sugar
- Why Belly Fat Increases with Aging
- Aging T1D & Muscle Loss
- Ashley McEvoy Sudden Announcement as New Insulet CEO
- Microdosing GLP-1s
- UHC’s Stock Drop
Sequel Med Tech, Senseonics to integrate year-long CGM into automated insulin delivery system by Sean Whooley for DrugDeliveryBusiness.com, 29 April 2025.
 Sequel Med Tech and Senseonics announced a commercial development agreement to combine insulin delivery and glucose monitoring systems. The companies plan to integrate Sequel’s twiist automated insulin delivery system with the Senseonics Eversense 365 continuous glucose monitor (CGM). This collaboration would make Twiist the first AID system compatible with Eversense 365, the world’s first and only one-year continuous glucose monitor (CGM). Sequel and Senseonics say they have already started their work to integrate the latest-generation, 365-day implantable sensor with Twiist. They expect to make the integrated offering available in the third quarter of this year.
Sequel Med Tech and Senseonics announced a commercial development agreement to combine insulin delivery and glucose monitoring systems. The companies plan to integrate Sequel’s twiist automated insulin delivery system with the Senseonics Eversense 365 continuous glucose monitor (CGM). This collaboration would make Twiist the first AID system compatible with Eversense 365, the world’s first and only one-year continuous glucose monitor (CGM). Sequel and Senseonics say they have already started their work to integrate the latest-generation, 365-day implantable sensor with Twiist. They expect to make the integrated offering available in the third quarter of this year.
“Sequel is committed to investing in innovations that empower people with diabetes with options in how they manage their diabetes,” said Sequel CEO and co-founder Dr. Alan Lotvin. “By partnering with Senseonics, a company pioneering long-duration CGM, we aim to deliver the flexibility people want to personalize their diabetes management on their terms.”
Read more: Sequel Med Tech, Senseonics to integrate year-long CGM into automated insulin delivery system
ADOCIA to Present New Data on AdoShell on Potential Curative Treatment for Type 1 Diabetes, shared on BusinessWire.com, 28 April 2025. New preclinical data support AdoShell islets’ progression toward First-In-Human clinical trial submission in 2025.
 ADOCIA announced that the latest preclinical data from its innovative AdoShell® technology platform has been selected for presentations at four upcoming scientific conferences. AdoShell® Islets is an innovative immunoprotective hydrogel designed to encapsulate pancreatic islets, with the goal of curing diabetes through cell therapy without requiring immunosuppression. This semi-permeable hydrogel allows the diffusion of insulin and glucose while preventing the infiltration of antibodies and immune cells that would lead to graft rejection.
ADOCIA announced that the latest preclinical data from its innovative AdoShell® technology platform has been selected for presentations at four upcoming scientific conferences. AdoShell® Islets is an innovative immunoprotective hydrogel designed to encapsulate pancreatic islets, with the goal of curing diabetes through cell therapy without requiring immunosuppression. This semi-permeable hydrogel allows the diffusion of insulin and glucose while preventing the infiltration of antibodies and immune cells that would lead to graft rejection.
The new data presented by Adocia notably discloses the success of the scale-up in delivering the therapeutic dose for the first in-human study, which is planned to be submitted to the regulatory authorities in 2025.
Read more: New Data on AdoShell Showing Potential Curative Treatment for T1D
The Best Way to Treat Hypoglycemia by Dan Heller for DanHeller.substack.com, 1 May 2025.
 GREAT POST/MUST READ on How To Treat a HYPO!!!
GREAT POST/MUST READ on How To Treat a HYPO!!!
It’s nearly impossible to properly know (or even estimate) the exact amount of glucose needed for a hypo event. Most people eat more than they need, which is understandable—hypoglycemia is akin to torture. Yet, over-compensation often leads to the dreaded glucose roller coaster: Sugars skyrocket too far, thereby requiring insulin to correct, which is also too much, and into the loop part of the roller coaster we go.
This article really narrows it down to one thing: the best way to treat it. But along the way, we also have to learn some physiological aspects about it, not just because it’ll help you better understand why the treatment works, but it will also unmask a lot of misunderstandings about hypos that may make you less afraid of it.
Everything you eat goes through a process called gastric emptying, which is characterized by the rate at which the stomach delivers its contents to the small intestine and how the body processes those contents.
In non-T1Ds, when glucose levels drop too low, the sympathetic nervous system responds in two ways: First, it accelerates gastric emptying, facilitating rapid glucose absorption. So, if someone (say, an athlete) runs low on glucose, they can slam down an energy gel and all’s well. Secondly, the sympathetic nervous system signals alpha cells (that sit next to beta cells) to produce glucagon, a hormone that signals the liver to produce glucose (gluconeogenesis), which raises glucose levels. To prevent blood glucose levels from bouncing around, the body synchronizes its insulin and glucagon secretion to be in tight communication. This is why the alpha and beta cells are physically next to each other in the pancreas—they talk to each other. This tight ecosystem of signaling is essentially how a non-T1D body maintains glucose levels.
But in T1D, the beta cells are dead, so this communication is broken, and it leads to a cascade of problems that, over time, waterfall into a progressively difficult state of affairs. The first thing that happens is that alpha cells never get a signal from beta cells, so the usual “trickle” of glucagon that rides alongside insulin doesn’t happen. As glucose levels begin to be more erratic and trend higher, it leads to neuropathy, particularly in the sympathetic nervous system. And since the sympathetic nervous system governs digestion, the “gastric emptying” process slows down in ways that are unpredictable and volatile, often without notice. When the condition surpasses a particular threshold, it’s classified as gastroparesis, a condition that affects approximately 28% of T1Ds, according to the paper, Prevalence of delayed gastric emptying in diabetic patients.
Making matters worse, gastric emptying can also be slowed by hypoglycemia. This is the biphasic nature of the intestine and the nerves that govern it—in non-T1Ds, hypoglycemia can increase gastric emptying, but when T1D sets in, the process can reverse, slowing down absorption. For T1Ds who already have some degree of neuropathy, hypoglycemia-induced slowed gastric emptying can range from 30–50%.
Big notation for T1D’s that do carb-counting: Yes, this is REALLY good and important. However, just because you’ve counted carbs, it doesn’t mean that you know how much of those carbs have been absorbed. If you use a T1D app that attempts to present how many carbs are “on board,” do not trust it.
Read more: The Best Way to Treat Hypoglycemia
Zucara Therapeutics Announces 2nd and Final Closing of US$25 Million Series B Financing by PRNewsWire.com, 1 May 2025.
 Zucara Therapeutics Inc., a diabetes life sciences company developing ZT-01, the first once-daily therapeutic to prevent hypoglycemia (low blood glucose levels) in people with diabetes, announced that it has completed the 2nd and final closing of its US$25 million Series B Financing. The T1D Fund: A Breakthrough T1D Venture, and other new investors invested a combined US$5 million to complete the Financing. As previously announced, strategic investor Sanofi and existing investor The Perceptive Xontogeny Venture Fund invested a combined US$20 million as part of the Financing’s first closing.
Zucara Therapeutics Inc., a diabetes life sciences company developing ZT-01, the first once-daily therapeutic to prevent hypoglycemia (low blood glucose levels) in people with diabetes, announced that it has completed the 2nd and final closing of its US$25 million Series B Financing. The T1D Fund: A Breakthrough T1D Venture, and other new investors invested a combined US$5 million to complete the Financing. As previously announced, strategic investor Sanofi and existing investor The Perceptive Xontogeny Venture Fund invested a combined US$20 million as part of the Financing’s first closing.
“We are thrilled to close our Series B financing, which will enable us to complete our Phase 2a clinical trial and the nonclinical activities to support a once-weekly version of ZT-01,” said Michael Midmer, CEO of Zucara. “As one of the largest disease-focused impact investing funds in the world, the T1D Fund focuses on funding therapies that have significant potential for clinical impact in Type 1 diabetes, so we are delighted to have their support.”
Read more: Zucara Therapeutics Announces Second and Final Closing of US$25 Million Series B Financing
MORE on GLP-1s
GLP 1s – One Class of Drugs with Many Different Names is another great episode by Dr. Jeremy Pettus and Dr. Steve Edelman for TCOYD.org,
 In this episode, Dr. Jeremy Pettus and Dr. Steve Edelman go head-to-head in a friendly face-off between two of the most talked-about medications in diabetes and weight management: Ozempic and Mounjaro. Both are part of the powerful GLP-1 class, but which one might be better for you? From A1C reduction and weight loss to heart and kidney protection, ease of use, side effects, and insurance coverage—Drs. E & P walk you through a category-by-category comparison. They bring the clinical data and their own real-world patient experience to help you understand the key differences (and similarities) between these leading therapies. Whether you’re managing type 2 diabetes, living with type 1, or exploring options for weight loss, this episode is designed to help you make an informed decision with your healthcare provider. Key Topics:
In this episode, Dr. Jeremy Pettus and Dr. Steve Edelman go head-to-head in a friendly face-off between two of the most talked-about medications in diabetes and weight management: Ozempic and Mounjaro. Both are part of the powerful GLP-1 class, but which one might be better for you? From A1C reduction and weight loss to heart and kidney protection, ease of use, side effects, and insurance coverage—Drs. E & P walk you through a category-by-category comparison. They bring the clinical data and their own real-world patient experience to help you understand the key differences (and similarities) between these leading therapies. Whether you’re managing type 2 diabetes, living with type 1, or exploring options for weight loss, this episode is designed to help you make an informed decision with your healthcare provider. Key Topics:
-
-
-
- How These Medications Work: Learn the difference between GLP-1 and dual agonist therapies
- A1C Reduction: See which drug leads to greater blood sugar improvements based on head-to-head clinical trials.
- Weight Loss: Discover how much weight patients lose on each medication—and why Mounjaro often shows stronger results.
- Heart Health: Understand which medication has FDA approval for cardiovascular protection and what’s still under investigation.
- Kidney Protection: Explore the latest studies showing Ozempic’s ability to slow kidney disease progression.
- Side Effects: Get practical tips on managing common GI side effects and why titration matters.
- Ease of Use: Compare how the pens work, dosing flexibility, and what may be easier for patients day to day.
- Sleep Apnea: Find out how Mounjaro earned a new indication for reducing sleep apnea severity, especially through weight loss.
- Access for Type 1s: Learn why these meds aren’t yet approved for T1D and how some patients are still getting them.
- Emerging Indications: Hear about new uses for these meds, including fatty liver, osteoarthritis, and even alcohol reduction.
- How to Choose: Get expert guidance on which medication may be right for you based on your goals and health needs.
-
-
**********************************************************************
Mounjaro vs Ozempic: Which One Is Right for You? by TCOYD for TCOYD.org, 21 February 2025.
 Ozempic made a splashy debut in 2017 with a catchy jingle and celebrity following, and Mounjaro came onto the scene five years later as another impressive type 2 diabetes medication that delivers impactful glucose management results along with significant weight loss. How are these two game-changing medications alike? How are they different? How do you know which one would be right for you?
Ozempic made a splashy debut in 2017 with a catchy jingle and celebrity following, and Mounjaro came onto the scene five years later as another impressive type 2 diabetes medication that delivers impactful glucose management results along with significant weight loss. How are these two game-changing medications alike? How are they different? How do you know which one would be right for you?
-
-
- Ozempic and Mounjaro are injectable type 2 diabetes medications that help control blood sugars and promote weight loss.
- Ozempic mimics a hormone in the body called GLP-1 RA, and Mounjaro mimics the GLP-1 RA and the GIP hormones. Your stomach releases these hormones after eating to stimulate insulin secretion, reduce glucose production in the liver, and slow stomach motility.
- Ozempic and Mounjaro are diabetes medications that help improve glucose control and aid in weight loss. Both medications are highly effective, but Mounjaro’s dual mechanism may offer more potent effects on blood sugar and weight reduction.
- Both semaglutide (the main ingredient in Ozempic) and tirzepatide (the main ingredient in Mounjaro) are being studied for several additional health benefits.
-
**********************************************************************
Semaglutide effectively treats liver disease in two-thirds of patients, according to King’s College, London for MedicalXpress.com, 30 April 2025.
 Results from the ESSENCE Phase III clinical trial published in the New England Journal of Medicine show that treating patients with semaglutide can halt and even reverse liver disease. The placebo-controlled outcome trial of participants with a life-threatening form of liver disease known as metabolic dysfunction-associated steatohepatitis (MASH) was conducted at 253 clinical sites across 37 countries around the world. This is the first regulatory-level trial showing the benefit of semaglutide for people with MASH.
Results from the ESSENCE Phase III clinical trial published in the New England Journal of Medicine show that treating patients with semaglutide can halt and even reverse liver disease. The placebo-controlled outcome trial of participants with a life-threatening form of liver disease known as metabolic dysfunction-associated steatohepatitis (MASH) was conducted at 253 clinical sites across 37 countries around the world. This is the first regulatory-level trial showing the benefit of semaglutide for people with MASH.
The trial is led by two chief investigators, Professor Philip Newsome at King’s College London and Arun Sanyal at the VCU School of Medicine, United States. Researchers also found other benefits. Those receiving semaglutide also saw improvements in liver enzymes and other blood measures of liver fibrosis, as well as 10.5% weight loss.
**********************************************************************
How GLP-1s Could Help People Sleep Better — Beyond Weight Loss by Jayne Jacova Feld for EndocrinologyAdvisor.com, 25 April 2025.
In addition to promoting weight loss, GLP-1 receptor agonists may improve sleep apnea through their anti-inflammatory effects, which could play a key role in reducing airway obstruction and enhancing overall sleep quality. Chronic low-grade inflammation is a common issue among people with obesity and sleep apnea, contributing to airway swelling and frequent breathing interruptions during the night. The root of this inflammation often stems from a vicious cycle tied to OSA itself, Dr Malhotra explains.
GLP-1 receptor agonists’ impact on sleep may also be tied to their ability to regulate energy metabolism and stabilize glucose levels. Sleep and metabolism are closely intertwined, as the body’s circadian rhythms help to regulate both processes. Disruptions in one system can spill over into the other, which is why people with conditions like type 2 diabetes often experience poor sleep.
Another intriguing benefit is the medication’s potential to improve mental health. Study findings have shown GLP-1 receptor antagonists can reduce anxiety and depression, likely due to their effects on neurotransmitters and inflammatory pathways in the brain.
Read more: How GLP-1s Could Help People Sleep Better — Beyond Weight Loss
This Is Your Body on Sugar by Alice Callahan for NYTimes.com, 30 October 2024.
How much sugar is too much? Federal health officials recommend that no more than 10 percent of your daily calories come from added sugars. If you consume 2,000 calories per day, this works out to no more than 50 grams of added sugars per day. The American Heart Association sets a stricter limit of 6 percent of calories consumed, or no more than about 25 grams per day for women & 36 grams per day for men. On average, people in the United States consume about 67 grams of added sugars per day.
Read more: This Is Your Body on Sugar
Why our waistlines expand in middle age—aging stem cells shift into overdrive by City of Hope National Medical Center for MedicalXpress.com, 25 April 2025.
 Belly fat accelerates aging and slows down metabolism, increasing our risk for developing diabetes, heart problems, and other chronic diseases. Exactly how age transforms a six-pack into a softer stomach, however, is unclear. Now, preclinical research by City of Hope has identified the cellular culprit behind age-related abdominal fat, offering new insights into why our midsections tend to widen with middle age. Published today in Science, the findings suggest a novel target for future therapies to prevent belly flab and extend our healthy lifespans.
Belly fat accelerates aging and slows down metabolism, increasing our risk for developing diabetes, heart problems, and other chronic diseases. Exactly how age transforms a six-pack into a softer stomach, however, is unclear. Now, preclinical research by City of Hope has identified the cellular culprit behind age-related abdominal fat, offering new insights into why our midsections tend to widen with middle age. Published today in Science, the findings suggest a novel target for future therapies to prevent belly flab and extend our healthy lifespans.
“People often lose muscle and gain body fat as they age—even when their body weight remains the same,” said Qiong (Annabel) Wang, Ph.D., the study’s co-corresponding author and an associate professor of molecular and cellular endocrinology at City of Hope’s Arthur Riggs Diabetes & Metabolism Research Institute. “We discovered aging triggers the arrival of a new type of adult stem cell and enhances the body’s massive production of new fat cells, especially around the belly.”
While it’s well-known that fat cells grow larger with age, scientists suspected that white adipose tissue (WAT), the fatty tissue responsible for age-related weight gain, also expands by producing new fat cells, suggesting it may have an unlimited potential for growth. Aging also transformed the APCs into a new type of stem cell, called age-specific committed preadipocytes (CP-As). Arising in middle age, CP-A cells actively produce new fat cells, explaining why older mice tend to gain more weight. A signaling pathway, specifically the leukemia inhibitory factor receptor (LIFR), proved critical for promoting the multiplication and evolution of these CP-A cells into fat cells.
Read more: Why our waistlines expand in middle age—aging stem cells shift into overdrive
Diabetes, Aging, and Muscle Loss: What You Need To Know by Amelia Harnish for diaTribe.org, 29 January 2024.
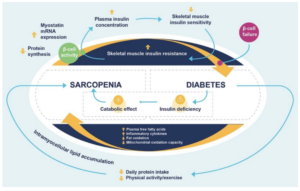 Recent research has found a strong link between diabetes and sarcopenia, otherwise known as accelerated age-related muscle loss. The study also found that people with diabetes have three times the risk of sarcopenia compared to those without diabetes. Sarcopenia in older adults is associated with an increased risk of falls, frailty, and mortality. As people with diabetes live longer – more than a quarter of Americans 65 or older have diabetes – this complication is increasingly on clinicians’ radars.
Recent research has found a strong link between diabetes and sarcopenia, otherwise known as accelerated age-related muscle loss. The study also found that people with diabetes have three times the risk of sarcopenia compared to those without diabetes. Sarcopenia in older adults is associated with an increased risk of falls, frailty, and mortality. As people with diabetes live longer – more than a quarter of Americans 65 or older have diabetes – this complication is increasingly on clinicians’ radars.
If you live with diabetes, it should be on your radar, too, said Dr. Betul Hatipoglu, assistant professor and director of the Case Center for Diabetes, Obesity, and Metabolism at Case Western Reserve University in Ohio. “Sarcopenia is more common in older individuals who are at risk for muscle loss naturally. However, even younger people with diabetes could suffer from this side effect if not well-managed for a long time,” Hatipoglu said.
While some muscle loss is expected, sarcopenia is a swift rate of loss. Sarcopenia involves a loss of muscle mass, as well as a reduction in the function and strength of the muscles. As muscle mass decreases, fat mass increases, which increases the risk of insulin resistance. Diabetes and muscle loss seem to be a two-way street; not only does the condition seem to lead to muscle loss, but muscle loss itself can also lead to diabetes.
Sarcopenia can make diabetes more complicated to manage, in addition to other adverse effects like joint stiffness and decreased bone density. This can lead to a snowball effect where sarcopenia, combined with diabetes, speeds up overall health decline as you age.
Read more: Diabetes, Aging, and Muscle Loss: What You Need To Know
Ashley McEvoy named Insulet CEO by Elise Reuter for MedTechDive.com, 28 April 2025.
 Insulet has named Ashley McEvoy as CEO. The high-profile medical device executive, who led Johnson & Johnson’s medical technology business for several years, has been tasked with driving continued growth at the insulin pump maker. After nearly three years with the company, former CEO Jim Hollingshead resigned from his role and from Insulet’s board on 4/28/2025. Hollingshead will remain as a consultant for an undisclosed period.
Insulet has named Ashley McEvoy as CEO. The high-profile medical device executive, who led Johnson & Johnson’s medical technology business for several years, has been tasked with driving continued growth at the insulin pump maker. After nearly three years with the company, former CEO Jim Hollingshead resigned from his role and from Insulet’s board on 4/28/2025. Hollingshead will remain as a consultant for an undisclosed period.
Insulet’s board mutually agreed with Hollingshead that now is the right time to implement the leadership transition, the company said. While the firm was “surprised by the suddenness of the announcement,” a meeting with Insulet’s investor relations team confirmed the decision was related to succession planning and had nothing to do with Hollinghead’s performance. Hollingshead stepped into the CEO role in 2022 after former leader Shacey Petrovic left for personal reasons. He had been on Insulet’s board since 2019.
Read more: Ashley McEvoy named Insulet CEO
Microdosing GLP-1 medications: A new weight-loss trend? by Jean Lee for Tebra.com, 15 April 2025.
 Tebra surveyed 640 GLP-1 users about their experiences with microdosing. For private practices using EHR systems to manage chronic care and medication adherence, understanding why patients are microdosing, how they’re doing it, and what outcomes they’re experiencing is critical. This insight can help providers better anticipate patient behaviors, address concerns, and guide treatment plans.
Tebra surveyed 640 GLP-1 users about their experiences with microdosing. For private practices using EHR systems to manage chronic care and medication adherence, understanding why patients are microdosing, how they’re doing it, and what outcomes they’re experiencing is critical. This insight can help providers better anticipate patient behaviors, address concerns, and guide treatment plans.
-
-
- 36% of GLP-1 users are currently microdosing their medication.
- Nearly 1 in 4 GLP-1 microdosers (24%) have been microdosing for 6 months or more.
- TikTok is most often where people first learn about microdosing GLP-1s.
- More than 1 in 3 GLP-1 users (38%) are microdosing their medication to save money.
- Over 1 in 5 GLP-1 users who have microdosed (22%) regret doing so.
- Over 1 in 2 GLP-1 users who have microdosed have felt discouraged or shamed for doing so, and 14% by their doctor.
-
Read more: Microdosing GLP-1 medications: A new weight-loss trend?
What UnitedHealth’s Stock Drop Reveals About Medicare Advantage by N. Adam Brown for MedPageToday.com, 29 April 2025.
 UnitedHealth Group’s (UHG) share price recently plummeted by more than 22%, its steepest one-day drop in over a quarter century. At its core, the culprit wasn’t a scandal or a market-wide collapse. It was something far more revealing: patients started using more healthcare. Increased care utilization among Medicare Advantage members led to a worse-than-expected first quarter for UHG and cuts to its 2025 forecast. During a company earnings call, CEO Andrew Witty described the financial performance as “unusual and unacceptable” and argued that the problem was fixable. That should raise alarm bells.
UnitedHealth Group’s (UHG) share price recently plummeted by more than 22%, its steepest one-day drop in over a quarter century. At its core, the culprit wasn’t a scandal or a market-wide collapse. It was something far more revealing: patients started using more healthcare. Increased care utilization among Medicare Advantage members led to a worse-than-expected first quarter for UHG and cuts to its 2025 forecast. During a company earnings call, CEO Andrew Witty described the financial performance as “unusual and unacceptable” and argued that the problem was fixable. That should raise alarm bells.
His word choice says everything. When you break it down, he seems to imply that patients accessing care is a problem — a cost that hinders company performance. Witty indirectly acknowledged what we all know but is antithetical to making America healthy again: insurers are rewarded when care is avoided, delayed, or denied. When customers visit the doctor, undergo diagnostic tests, or access specialist care, insurers get worried because their profitability begins to decline.
Medicare Advantage is marketed as a private alternative to traditional Medicare. At its core, however, it is a redirection of tax dollars allocated to Medicare for the management of Medicare beneficiaries to private insurance companies.
Insurers receive a fixed monthly payment per patient known as the per-member-per-month (PMPM) rate. That money is meant to cover the same medical expenses for the individual that Medicare would traditionally cover, and sometimes more. If the insurer spends less than the PMPM, they keep the difference as profit. If they spend more, they absorb the loss. That is what happened to UHG.
In other words, as Medicare Advantage is structured, UHG and other participating insurers have an incentive to reduce the amount of care delivered. The only constraining factor is the need to avoid breaching federal quality and access requirements. While Medicare Advantage’s program goals are to contain costs and improve access, research suggests it may negatively impact care quality by making networks too narrow, reducing access to specialty care services, and eroding patient satisfaction.
Read more: What UnitedHealth’s Stock Drop Reveals About Medicare Advantage





It was only a matter of time before Senseonics and a pump company paired up. But here is the question: will the Senseonics sensor signal reach the pump when it is on the other side of the body? Medt cannot, Dexcom cannot, can Senseonics do it?
Is it possible that insurance providers are finding that when people use insurance, the less profitable they are? Who knew?
ADOCIA sounds interesting.