In this week’s issue of The Savvy Diabetic:
-
- Aspartame Triggers Insulin Spike
- Gut bacteria Alters Brain Proteins
- Rising World Diabetes Prevalence
- Medtronic Pump Air Travel Warning
- FTC Case Against PBMs Move Forward
- Happy Doctors = Practice Autonomy
- Sage Diabetes T1D Self-Care Collective
Artificial sweetener triggers insulin spike, leading to blood vessel inflammation in mice from Cell Press and published by MedicalXpress.com, 19 February 2025.
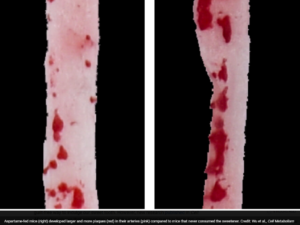 New research published in Cell Metabolism shows that aspartame, one of the most common sugar substitutes, may impact vascular health. The team of cardiovascular health experts and clinicians found that aspartame triggers increased insulin levels in animals, which in turn contributes to atherosclerosis—a buildup of fatty plaque in the arteries, which can lead to higher levels of inflammation and an increased risk of heart attacks and stroke over time.
New research published in Cell Metabolism shows that aspartame, one of the most common sugar substitutes, may impact vascular health. The team of cardiovascular health experts and clinicians found that aspartame triggers increased insulin levels in animals, which in turn contributes to atherosclerosis—a buildup of fatty plaque in the arteries, which can lead to higher levels of inflammation and an increased risk of heart attacks and stroke over time.
The research was inspired by a can of diet soda during a project meeting. “One of my students was sipping on this sugar-free drink, and I said, ‘Why don’t you look into that?'” recalls senior author Yihai Cao, who studies chronic diseases related to blood vessel disorders at Karolinska Institute in Sweden. Previous research has linked consumption of sugar substitutes to increased chronic disorders like cardiovascular disease and diabetes. However, the mechanisms involved were previously unexplored. Compared to mice without a sweetener-infused diet, aspartame-fed mice developed larger and more fatty plaques in their arteries and exhibited higher levels of inflammation, both of which are hallmarks of compromised cardiovascular health.
When the team analyzed the mice’s blood, they found a surge in insulin levels after aspartame entered their system. The team noted that this wasn’t a surprising result, given that our mouths, intestines, and other tissues are lined with sweetness-detecting receptors that help guide insulin release. But aspartame, 200 times sweeter than sugar, seemed to trick the receptors into releasing more insulin. They investigated how exactly elevated insulin levels lead to arterial plaque buildup and identified an immune signal called CX3CL1 that is especially active under insulin stimulation.
“Because blood flow through the artery is strong and robust, most chemicals would be quickly washed away as the heart pumps,” says Cao. “Surprisingly, not CX3CL1. It stays glued to the surface of the inner lining of blood vessels. There, it acts like a bait, catching immune cells as they pass by.” Many of these trapped immune cells are known to stoke blood vessel inflammation. However, when researchers eliminated CX3CL1 receptors from one of the immune cells in aspartame-fed mice, the harmful plaque buildup didn’t occur. These results point to CX3CL1’s role in aspartame’s effects on the arteries, says Cao.
Read more: Artificial sweetener triggers insulin spike, leading to blood vessel inflammation in mice
Gut bacteria can alter brain proteins: New glycosylation method uncovers link by Shreya Ghosh for Phys.org, 10 February 2025.
 A new study from EMBL Heidelberg researchers shows that gut bacteria can bring about profound molecular changes in one of our most critical organs—the brain. The new study, published in the journal Nature Structural & Molecular Biology, is the first to show that bacteria living in the gut can influence how proteins in the brain are modified by carbohydrates—a process called glycosylation. The study was made possible by a new method the scientists developed—DQGlyco—which allows them to study glycosylation at a much higher scale and resolution than previous studies.
A new study from EMBL Heidelberg researchers shows that gut bacteria can bring about profound molecular changes in one of our most critical organs—the brain. The new study, published in the journal Nature Structural & Molecular Biology, is the first to show that bacteria living in the gut can influence how proteins in the brain are modified by carbohydrates—a process called glycosylation. The study was made possible by a new method the scientists developed—DQGlyco—which allows them to study glycosylation at a much higher scale and resolution than previous studies.
Proteins are the workhorses of our cells and their main building blocks. Sugars, or carbohydrates, on the other hand, are among the body’s main sources of energy. However, the cell also uses sugars to chemically modify proteins, altering their functions. This is called glycosylation.
“Glycosylation can affect how cells attach to each other (adhesion), how they move (motility), and even how they talk to one another (communication),” explained Clément Potel, first author of the study and Savitski Team Research Scientist. “It is involved in the pathogenesis of several diseases, including cancer and neuronal disorders.”
DQGlyco uses easily available and low-cost laboratory materials, such as functionalized silica beads, to selectively enrich glycosylated proteins from biological samples, which can then be precisely identified and measured. Applying the method to brain tissue samples from mice, the researchers could identify over 150,000 glycosylated forms of proteins (‘proteoforms’), an increase of over 25-fold compared to previous studies. The quantitative nature of the new method means that researchers can compare and measure differences between samples from different tissues, cell lines, species etc. This also allows them to study the pattern of ‘microheterogeneity’—the phenomenon where the same part of a protein can be modified by many (sometimes hundreds of) different sugar groups.
Read more: Gut bacteria can alter brain proteins: New glycosylation method uncovers link
Rising diabetes prevalence in low-income countries ‘alarming and discouraging’ by Michael Monostra for Healio.com/endocrinology, 17 February 2025.
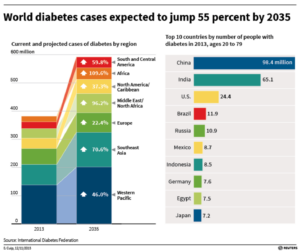 The prevalence of diabetes is increasing faster in some low-income countries than elsewhere in the world, generating concerns about healthcare infrastructure and access to treatment for people in those regions.
The prevalence of diabetes is increasing faster in some low-income countries than elsewhere in the world, generating concerns about healthcare infrastructure and access to treatment for people in those regions.
In November, the WHO Collaborating Centre for Noncommunicable Disease (NCD) Surveillance, Epidemiology and Modelling published a study in The Lancet with estimates of the global diabetes prevalence and treatment coverage from 1990 to 2022. The researchers concluded that approximately 828 million adults worldwide had diabetes in 2022, which was an increase from an estimated 630 million adults with diabetes in 1990.
The rising prevalence of diabetes is especially challenging for lower-income countries, as many do not have a healthcare infrastructure that is as robust as higher-income nations, according to Leonard Egede, MD, MS, the Charles and Mary Bauer Endowed Chair and professor of medicine at Jacobs School of Medicine and Biomedical Sciences at University at Buffalo and president and CEO of UBMD Internal Medicine.
“I break it down into three main challenges,” Egede said. “One is having enough providers to provide care. Because these areas are remote, things like screening and clinical care become more difficult. The second is testing and treatment challenges. When you live in environments where transportation is challenging, getting supplies like test strips, medications and even [food] is a challenge. Third is financial challenges. [Lower-income] countries are financially challenged or not very well-resourced. Diabetes then puts a huge burden on the economy.”
Read more: Rising diabetes prevalence in low-income countries ‘alarming and discouraging’
Medtronic Warns About Insulin Pump Action During Air Travel by Miriam E. Tucker for MedScape.com, 19 February 2025.
 Medtronic has issued an “Urgent Medical Device Correction” about the accuracy of insulin pump delivery during changes in air pressure, such as airplane takeoffs and landings. “We request you share with these patients a communication that Medtronic created to inform them of the importance of monitoring their glucose levels during dynamic atmospheric pressure conditions – such as flight takeoff and flight landing, as insulin delivery volume accuracy may be impacted,” the company said in the alert.
Medtronic has issued an “Urgent Medical Device Correction” about the accuracy of insulin pump delivery during changes in air pressure, such as airplane takeoffs and landings. “We request you share with these patients a communication that Medtronic created to inform them of the importance of monitoring their glucose levels during dynamic atmospheric pressure conditions – such as flight takeoff and flight landing, as insulin delivery volume accuracy may be impacted,” the company said in the alert.
Products covered by the alert include the MiniMed Paradigm, MiniMed 600 series (640G, 670G) and MiniMed 700 series (770G, 780G) insulin pumps. However, insulin pump over- and under-delivery with atmospheric change isn’t unique to Medtronic’s products, as Medscape Medical News reported in 2024 and in 2016. The phenomenon was described in the literature in 2011.
Unintended insulin delivery can occur with expansion of air bubbles inside the reservoir when the air pressure decreases, as with flight takeoff, potentially leading to hypoglycemia. This can occur even when the pump’s delivery is suspended or programmed to zero units per hour, Medtronic cautioned. And when air pressure increases, as with airplane landing, the air bubbles can be compressed and result in less insulin being delivered than intended, leading to hyperglycemia.
Read more: Medtronic Warns About Insulin Pump Action During Air Travel
FTC case against Caremark, Express Scripts, Optum Rx can move forward, judge rules by Rebecca Pifer for HealthCareDive.com, 20 February 2025.
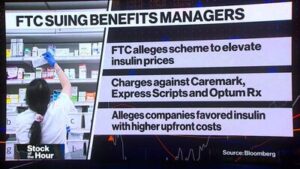 The FTC’s lawsuit against Caremark, Express Scripts and Optum Rx — known as the “Big Three” PBMs for their outsized control of the U.S. prescription market — hinges on allegations the drug middlemen prefer more expensive insulin products to generate higher rebates in negotiations with drugmakers. That preference drives drugmakers to increase the list price of their medications, raising costs for payers and consumers down the line, according to the FTC.
The FTC’s lawsuit against Caremark, Express Scripts and Optum Rx — known as the “Big Three” PBMs for their outsized control of the U.S. prescription market — hinges on allegations the drug middlemen prefer more expensive insulin products to generate higher rebates in negotiations with drugmakers. That preference drives drugmakers to increase the list price of their medications, raising costs for payers and consumers down the line, according to the FTC.
Caremark, Express Scripts and Optum Rx deny their practices contribute to higher prices, and characterize the FTC’s suit as the culmination of top antitrust regulators’ crusade against the PBM industry. The Big Three also say how the FTC lodged its suit — in an in-house administrative court, instead of a federal one — is unconstitutional, as it allows the agency to act both as a prosecutor and a judge.
Judge Matthew Schelp of the U.S. District Court for the Eastern District of Missouri was unswayed by their point of view. The PBMs’ arguments don’t have enough merit to throw out the case entirely at this premature stage, Schelp wrote in an order filed. The PBMs also haven’t shown irreparable harm to warrant a preliminary injunction — and, case precedent shows that the FTC’s adjudicative functions don’t deny due process, Schelp found.
An injunction now would be “against the public’s interest,” Schelp said.
Read more: FTC case against Caremark, Express Scripts, Optum Rx moves forward
Want happier doctors? Restoring their practice autonomy is a must by Georgia Garvey for AMA-Assn.org, 18 February 2025.
So, what is Type 1 Diabetes? by Mandy Jones for SageDiabetes.co, a heart-centered support for the T1D journey.
 The Physical Answer: I could give the scientific explanation. You know that one… Type 1 Diabetes (T1D) is an autoimmune condition in which the pancreas no longer produces insulin. Managing it means calculating the right amount of insulin based on carbohydrate intake at every meal. But this answer barely scratches the surface. It tells the other person nothing about what it feels like to live with T1D—and what makes it so challenging.
The Physical Answer: I could give the scientific explanation. You know that one… Type 1 Diabetes (T1D) is an autoimmune condition in which the pancreas no longer produces insulin. Managing it means calculating the right amount of insulin based on carbohydrate intake at every meal. But this answer barely scratches the surface. It tells the other person nothing about what it feels like to live with T1D—and what makes it so challenging.
The Emotional Answer: The real answer is in the tears, the anxiety, the grit, the constant calculations, and the cognitive load that never lets up. I’ve been trying to speak to this one instead, because I feel it gives people a better understanding of me, my challenges, and why I’ve been pouring my time into this project at Sage Diabetes. I think T1D is one of the top five most demanding chronic illnesses in terms of self-management. Many conditions—hypothyroidism, even cancer—are treated with set medication doses prescribed by a doctor. But with T1D, there is no fixed dose. We are our own nurses, deciding how much medication to give ourselves, at least 5-15 times a day.
The Complexity of Insulin: The complexity of insulin is that it’s not just any medication—it’s a hormone that interacts with every other hormone in our body. How much we need changes constantly, depending on stress levels, exercise, time of day, time of the month. What worked yesterday might not work today. Healthcare professionals hand us equations and ratios, but life isn’t a formula—it’s a dance. Managing T1D is an art form, and must be danced with, moment to moment, ever-changing and always in flux. On top of that, I say bluntly, that insulin is potentially lethal. That fact is not lost on us. The fear of a big error in those calculations
Pressure Creates Diamonds: Diamonds are formed through pressure, and so are all us fierce, tender Type 1’s. These constant pressure points in T1D force us to recalibrate, and offer us an opportunity to:
-
-
- To come back into moment-to-moment communication with our bodies, in a world so often dominated by the mind.
- To examine our cultural relationship with perfectionism.
- To redefine our narratives about success and failure.
- To rethink what it means to take care of ourselves—what actually supports us versus what we think “should” work.
- To learn the landscape of our nervous systems —so we can feel resilient more often than we feel caught off-guard.
-
 Mandy shared: “That’s why I wanted to create the T1D Self-Care Collective—a space to unpack these questions, support each other, and build a new kind of resilience. If this resonates with you, I’d love to have you join. Curious? Send me an email Mandy Jones (mandy@sagediabetes.co) with the subject, ‘I’m Curious’ and I’ll share more details about the sweet lil’ group.”
Mandy shared: “That’s why I wanted to create the T1D Self-Care Collective—a space to unpack these questions, support each other, and build a new kind of resilience. If this resonates with you, I’d love to have you join. Curious? Send me an email Mandy Jones (mandy@sagediabetes.co) with the subject, ‘I’m Curious’ and I’ll share more details about the sweet lil’ group.”
Read more: Sage Diabetes: a soft place to rest in a messy healthcare system



Re: Aspartame: The mice were fed either aspartame or NO sweetened food. No one has a diet that has no sugars in food. Further, aspartame was found to trigger CX3CL1, a signaling molecule that influences insulin secretion. So does sugar. In fact, MORE SO. The ratio of aspartame in a normal diet relative to glucose is minor.
Most importantly, this only happens for those with working beta cells. None of this applies to T1Ds. You can eat all the aspartame you like, and you’re not going to get cardiovascular disease.
Aspartame was found to trigger CX3CL1, a signaling molecule that influences insulin secretion. So does sugar. In fact, MORE SO. The ratio of aspartame in a normal diet relative to glucose is minor.
Most importantly, this only happens for those with working beta cells. None of this applies to T1Ds. You can eat all the aspartame you like, and you’re not going to get cardiovascular disease.
I’ll be publishing a longer, more comprehensive article about sweeteners in my substack soon.
Can you please share any research article on this topic? The part about it not applying to folks without working beta cells … fascinating and why? Thanks Dan!
I will be publishing an article focused on this whole topic of artificial sweeteners very soon on my substack — it’s next in the queue. This research has been gaining too much attention to not address it. danheller.substack.com
I posted my article that addresses this study. I would highly encourage you to post it to your community to correct the misimpression that (clearly) some people had. The study is sensationalist and flawed. But, there are great lessons we can learn from one part of the study that is highly understated that most people are unaware of: Excess insulin levels can lead to heart disease, which is why type 1 and type 2 diabetics have shorter lifespans.
Such a good blog post, thank you!
Aspartame has long been suspected of causing bad outcomes in the human body. But, I also know I have been using it or other artificial for over 50 years. I don’t see myself giving it up based on this research. I am not even sure I can at this point. I must rely on the rapidly depleting public health system. No doubt in my lifetime this will not be resolved. I pray it will be in the future.
The litigation against Caremark is one of the best things happening right now. I purchased one of the first PBM’s used in a plan for police and fire personnel. It was revolutionary for our plan and saved much money in the first year.
But slowly plans lost control of PBM’s instead of the plan controlling the PBM, the PBM controlled the plans. That was due in large part to the cost of medication and its use.
My first plan was primarily controlled by hospital and doctor costs, which are today almost insignificant. Instead, the cost of health insurance is largely determined by medication and outpatient services. The PBM is the most significant part of the plan’s cost.
Yet PBM’s are little more than black boxes, money goes in and drugs pour out. What was stated as a way to save the plan money is today a method of creating profit for PBM, the most critical example I know is the cost of insulin. PBM’s added significant “bribe” shakedown money to the price of the drug until the average person cannot afford it and the plans were being charged arbitrary fees.
It took the issue of non-name brand insulin produced on the same lines as typical insulin and priced hundreds of dollars per vial less than the price controlled by the PBM. The PBMs were shown to be the cause of jacked up process, created by the PBM
We may suggest that the cost of name-brand insulin is too high, but we cannot argue that PBMs were profiting about $200.00 per vial from the cost of insulin. Then they would tell the plan providers, “Look how much we saved you. ” Since they take half, they never disclosed that they were the reason for the increase in prices.
In my opinion, it was no more or less than legal extortion, and I suspect this is replicated across hundreds of medications. Insulin was just the most public example. Terrible.
While the plan was being shown these inflated savings, the non-plan users were paying an exorbitant price. By contract, the manufacturer could not lower the price, so they produced a new biosimilar ( it is the same product) and labeled it as such.
The PBM gig was up, and they purchased the biosimilar named product and showed that they were reducing the inflated price they were charging plans. In other words, the PBM was completely out of control and no longer working to lower costs; they were significantly raising prices.
The PBM’s should, in my opinion, face great legal jeopardy for their action in the last 15 years. Just my opinion. Now will the new FDA pursue this litigation? It isn’t very likely..