In this week’s issue of The Savvy Diabetic:
-
-
Warning about SmartPhone Alert Settings
-
rBio Addresses Insulin Shortages
-
GlucoTrack Trial Success
-
Yo-Yo Dieting & Kidney Damage
-
Insulin Pump BACKUP Plan (video)
-
Beta Bionics iLet Upgrades (video)
-
Fake Research Papers
-
GAD Antibodies & T1D
-
Pebble Watch is Back
-
DIY Insulearner App
-
3-Second Slices of Joy
-
FDA Warns About Diabetes Device Smartphone Alert Settings by Miriam E. TUcker for MedScape.com, 6 February 2025.
 The US Food and Drug Administration (FDA) is cautioning patients and caregivers about the potential for not receiving blood glucose level alerts from diabetes-related smartphone devices due to improper setting configurations, particularly following software or hardware updates.
The US Food and Drug Administration (FDA) is cautioning patients and caregivers about the potential for not receiving blood glucose level alerts from diabetes-related smartphone devices due to improper setting configurations, particularly following software or hardware updates.
On February 5, 2025, the FDA issued an alert it has received reports of missed alarms for patients who use continuous glucose monitors (CGMs), insulin pumps, or automated insulin delivery systems. Whether the alarm didn’t occur or wasn’t heard, the result can lead to harm from extremes of hypoglycemia or hyperglycemia.
Healthcare providers are advised to inform patients and their caregivers who rely on smartphone-connected diabetes devices to periodically check the smartphone settings to ensure critical alerts can be delivered. Such checks should also be conducted following any hardware or software updates or connecting any external software to make sure the device can still issue alerts.
Specific problems cited by the FDA include use of app “do not disturb” or “focus mode” configurations that prevent alarms, or the app entering a “deep sleep” after a period of disuse. In addition, connecting new hardware such as wireless earphones or car audio can change default alert volumes.
Read more: FDA Warns About Diabetes Device Smartphone Alert Settings
As Major Insulin Producers Shift Focus, rBIO Steps Up to Address Potential Shortages by PRNewsWire.com, 4 February 2025.
 Recent price cuts by major insulin manufacturers may appear to address affordability challenges, but they primarily target older insulin drugs nearing patent expiration. This tactic, coupled with the discontinuation of essential insulins like Novo Nordisk Levemir® and a shift in focus towards more profitable GLP-1 drugs, creates a concerning landscape of potential shortages and continued high costs for many patients.
Recent price cuts by major insulin manufacturers may appear to address affordability challenges, but they primarily target older insulin drugs nearing patent expiration. This tactic, coupled with the discontinuation of essential insulins like Novo Nordisk Levemir® and a shift in focus towards more profitable GLP-1 drugs, creates a concerning landscape of potential shortages and continued high costs for many patients.
rBIO, a biotechnology company committed to improving insulin access and affordability, is stepping up to fill this gap. Today, the company announced the successful completion of preclinical studies for its first biosimilar insulin, R-biolin, demonstrating bioequivalence to Novolin® R. “While some celebrate price reductions on older insulins, the reality is that many patients rely on specific formulations that are being phased out or remain prohibitively expensive,” said Cameron Owen, CEO of rBIO. “Our mission is to ensure a stable supply of affordable insulin options, starting with our lead biosimilar, R-biolin, and continuing with our next project, a biosimilar to Levemir.”
“As a patient advocate, I’m deeply concerned about the industry’s focus on profits over patients,” said Alison Smart, founder of the Alliance to Protect Insulin Choice. “rBIO’s dedication to developing affordable biosimilars offers a much-needed solution to the challenges faced by the diabetes community.”
“We recognize the urgent need for a Levemir biosimilar and are committed to bringing a product to market as quickly as possible,” added Owen. “Our goal is to ensure that no patient is left without access to the insulin they need. With R-biolin now validated, we are looking for partners to help us achieve scale-up.”
Read more: As Major Insulin Producers Shift Focus, rBIO Steps Up to Address Potential Shortages
Glucotrack hits trial success for direct blood measuring CGM by GlobalData.com, 5 February 2025.
 Glucotrack has successfully completed a first-in-human study with its continuous glucose monitor (CGM) that directly measures glucose levels from a blood vessel.
Glucotrack has successfully completed a first-in-human study with its continuous glucose monitor (CGM) that directly measures glucose levels from a blood vessel.
The company’s system is placed in the subclavian vein, a blood vessel that runs under the collar bone bringing deoxygenated blood back to the heart. Glucotrack calls its device, which has no external on-body component, a continuous blood glucose monitor (CBGM). The implant is around the length and thickness of three US nickels, with a total volume of 2.5cc. This makes the device smaller than many implantable medical devices such as pacemakers, which have a volume of around 8cc.
Read more: Glucotrack hits trial success for direct blood measuring CGM
‘Yo-Yo Dieting’ Could Be Hard on Kidneys in Type 1 Diabetes Patients by Kristen Monaco for MedPageToday.com, 4 February 2025.
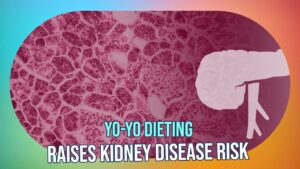 Body-weight cycling, sometimes referred to as yo-yo dieting, may be harmful to the kidneys for people with type 1 diabetes, according to retrospective data analysis.
Body-weight cycling, sometimes referred to as yo-yo dieting, may be harmful to the kidneys for people with type 1 diabetes, according to retrospective data analysis.
high variability of average body weight was associated with a 25% higher risk of experiencing a 40% decline in estimated glomerular filtration rate (eGFR) over an average 6-year follow-up (HR 1.25, 95% CI 1.09-1.41, P=0.001), reported Marion Camoin, MD, of Bordeaux University Hospital in France, and colleagues in the Journal of Clinical Endocrinology & Metabolism.
Greater weight variability also was associated with significantly higher risks for a few other negative renal outcomes, which were adjusted for several variables including baseline eGFR, HbA1c, and use of angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs). There was also a trend towards an increased risk for moderate albuminuria and severe albuminuria (>300 mg/24 hours), though this didn’t reach significance after adjustment.
“In type 1 diabetes, insulin therapy may play a particularly significant role in driving body-weight cycling due to the anabolic effects of the hormone,” Camoin and colleagues pointed out. “Weight loss can result from suboptimal insulin therapy, while weight gain is commonly associated with improved glycemic control. Additionally, the hypoglycemia risk associated with insulin use may lead to defensive snacking and reduced physical activity.”
Read more: ‘Yo-Yo Dieting’ Could Be Hard on Kidneys in Type 1 Diabetes Patients
WHAT’S YOUR BACKUP PLAN?
Insulin Pump Failure: A Diabetes-Pharmacist Explains Next Steps by Diana Isaacs for T1DExchange.org, February 2025.
 There are times, however, when insulin pumps malfunction or fail, just like any other technology. When this happens, a backup plan will come in handy — especially when it’s the middle of the night or you’re away from home. While calling the insulin pump company may provide an easy fix, you could also need a replacement pump, which means some waiting time. In other words, you’ll need a “plan B” for managing T1D while you’re waiting.
There are times, however, when insulin pumps malfunction or fail, just like any other technology. When this happens, a backup plan will come in handy — especially when it’s the middle of the night or you’re away from home. While calling the insulin pump company may provide an easy fix, you could also need a replacement pump, which means some waiting time. In other words, you’ll need a “plan B” for managing T1D while you’re waiting.
DO YOU KNOW HOW TO switch from your pump management to injections? If not, PLEASE talk with your healthcare provider and have a written plan for using multiple daily injections, using long-acting and short-acting insulin with a syringe, until your pump is back up and working!
Do you have the following on hand?
-
-
- Insulin syringes or pen needles
- Long-acting insulin (vial or pen) that’s not expired
- Ketone test strips (you can purchase these over the counter)
-
Part of your backup plan will be knowing what to do in case you have ketones in your urine. Your healthcare team will inform you about next steps, but if you’re ever in doubt, call them or seek emergency care. DKA can be a life-threatening condition.
Let’s take a closer look at the different types of long-acting insulin.
-
-
- Insulin glargine (Rezvoglar, Basaglar, Lantus, Semglee) is taken once daily, lasts about 24 hours in the body.
- Insulin degludec (Tresiba) is taken once daily, lasts about 42 hours in the body.
- Insulin glargine U-300 (Toujeo) is a more concentrated form of insulin glargine taken once daily, lasts about 36 hours.
- Insulin NPH (Novolin N and Humulin N) is an intermediate-acting insulin taken twice daily, lasts about 14 hours.
-
How do I know how much insulin to take? Talk to your healthcare team about your individual needs. Insulin needs vary from person to person. If you’re comfortable doing so, calculate a long-acting dose by looking at your pump’s average basal insulin dose. You can find this in the pump history menu or on a pump report. At each visit, you can ask your healthcare provider if the insulin amounts in your backup plan need updating and if you have an active prescription.
Read more: Insulin Pump Failure: A Diabetes-Pharmacist Explains Next Steps
Fake papers are contaminating the world’s scientific literature, fueling a corrupt industry and slowing legitimate lifesaving medical research by Frederik Joelving, Cyril Labbe, and Guillaume Cabanac for TheConversation.com, 29 January 2025.
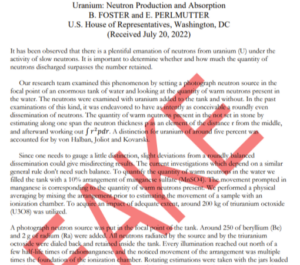 Over the past decade, furtive commercial entities around the world have industrialized the production, sale, and dissemination of bogus scholarly research, undermining the literature that everyone from doctors to engineers rely on to make decisions about human lives. It is exceedingly difficult to get a handle on exactly how big the problem is. Around 55,000 scholarly papers have been retracted to date, for a variety of reasons, but scientists and companies who screen the scientific literature for telltale signs of fraud estimate that many more fake papers are circulating – possibly as many as several hundred thousand. This fake research can confound legitimate researchers who must wade through dense equations, evidence, images, and methodologies only to find that they were made up.
Over the past decade, furtive commercial entities around the world have industrialized the production, sale, and dissemination of bogus scholarly research, undermining the literature that everyone from doctors to engineers rely on to make decisions about human lives. It is exceedingly difficult to get a handle on exactly how big the problem is. Around 55,000 scholarly papers have been retracted to date, for a variety of reasons, but scientists and companies who screen the scientific literature for telltale signs of fraud estimate that many more fake papers are circulating – possibly as many as several hundred thousand. This fake research can confound legitimate researchers who must wade through dense equations, evidence, images, and methodologies only to find that they were made up.
Even when the bogus papers are spotted – usually by amateur sleuths on their own time – academic journals are often slow to retract the papers, allowing the articles to taint what many consider sacrosanct: the vast global library of scholarly work that introduces new ideas, reviews other research, and discusses findings. The problem reflects a worldwide commodification of science. Universities, and their research funders, have long used regular publication in academic journals as requirements for promotions and job security, spawning the mantra “publish or perish.”
But now, fraudsters have infiltrated the academic publishing industry to prioritize profits over scholarship. Equipped with technological prowess, agility, and vast networks of corrupt researchers, they are churning out papers on everything from obscure genes to artificial intelligence in medicine.
Read more: Fake papers are contaminating the world’s scientific literature
GAD antibody testing and diabetes by Lize van der Walt for SweetLife.org and South Africans with Diabetes.
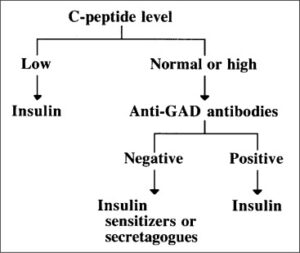 A GAD antibody test is a blood test that shows the presence of Glutamic Acid Decarboxylase antibodies, which are often used to diagnose Type 1 diabetes. About 75% of people with Type 1 diabetes have GAD antibodies.
A GAD antibody test is a blood test that shows the presence of Glutamic Acid Decarboxylase antibodies, which are often used to diagnose Type 1 diabetes. About 75% of people with Type 1 diabetes have GAD antibodies.
There have been longitudinal studies done to look at the relationship between enteroviruses and auto-immune disorders such as Type 1 diabetes for years (enteroviruses are a group of viruses and can affect many parts of the body, caused by any of several different viral strains). It has been found that children who were exposed to enteroviruses are more likely to develop Type 1 diabetes. However, this seems to disproportionately apply to children who carry a genetic variant in a surface protein of pancreatic beta cells.
GAD (glutamic acid dicarbon hydroxylase) is one of the substances involved in beta cell-specific auto-immune activation. In other words, the interstitial insulin production by pancreatic beta cells requires the enzyme GAD. Therefore, if for some reason the body produces specific anti-GAD antibodies against GAD, then the body will not be able to produce insulin, leading to a build-up of sugar in the blood.
GAD antibody testing determines which type of diabetes you have by measuring the concentration of antibodies against the GAD enzyme in the body. The GAD test is often used to assist in the diagnosis of Type 1 diabetes, determine whether gestational diabetes in pregnant women is Type 1 diabetes or not, and assess risk and monitor the progression of Type 1 diabetes.
75% of patients with Type 1 diabetes have anti-GAD antibodies in their blood, so the GAD antibody test is very important in classifying diabetes, thereby helping to choose the right treatment regimen for the patient. Anti-GAD antibodies may be present together with anti-insulin antibodies or may be the only antibodies in the patient’s blood. In addition, the Anti-GAD antibody test is also relevant to the prognosis of patients with future insulin-dependent transitions, which means it can predict whether or not someone will develop Type 1 diabetes. Although not when.
Read more: GAD antibody testing and diabetes
Why We’re Bringing Pebble Back by Eric Migicovsky on EricMigi.com, 27 January 2025.
 PebbleOS took dozens of engineers working over 4 years to build, alongside our fantastic product and QA teams. Reproducing that for new hardware would take a long time. Instead, we took a more direct route – I asked friends at Google (which bought Fitbit, which had bought Pebble’s IP) if they could open source PebbleOS. They said yes! Over the last year, a team inside Google (including some amazing ex-Pebblers turned Googlers) has been working on this. And today is the day – the source code for PebbleOS is now available at github.com/google/pebble. In addition to PebbleOS, we’ve been supporting development of Cobble, an open source Pebble-compatible app for iOS (soon) and Android.
PebbleOS took dozens of engineers working over 4 years to build, alongside our fantastic product and QA teams. Reproducing that for new hardware would take a long time. Instead, we took a more direct route – I asked friends at Google (which bought Fitbit, which had bought Pebble’s IP) if they could open source PebbleOS. They said yes! Over the last year, a team inside Google (including some amazing ex-Pebblers turned Googlers) has been working on this. And today is the day – the source code for PebbleOS is now available at github.com/google/pebble. In addition to PebbleOS, we’ve been supporting development of Cobble, an open source Pebble-compatible app for iOS (soon) and Android.
A small team and I are diving back into the world of hardware to bring Pebble back! This time round, we’re keeping things simple. Lessons were learned last time! I’m building a small, narrowly focused company to make these watches. The emphasis is on sustainability. I want to keep making cool gadgets and keep Pebble going long into the future.
Features:
-
- Always-on e-paper screen (it’s reflective rather than emissive. Sunlight readable. Glanceable. Not distracting to others.)
- Long battery life (one less thing to charge.)
- Simple and beautiful user experience (a core set of features I use regularly (telling time, notifications, music control, alarms, weather, calendar, sleep/step tracking)
- Buttons! (to play/pause/skip music on my phone without looking at the screen)
- Hackable (There were >16k watchfaces on the Pebble appstore!)
Do you have a hole in your heart (and on your wrist) that hasn’t been filled by any other smartwatch? Sign up to be the first to get one at rePebble.com.
Read more: Why We’re Bringing Pebble Back
NEW APP: Check out Insulearner, a new online OPEN SOURCE (not FDA approved) tool for computing insulin pump settings from diabetes data for people with Type 1 Diabetes.
 Insulearner uses a novel, data-driven approach for more personalized settings, leveraging first principles and modern machine learning techniques. It was created by Cameron Summers, a data scientist and dad of a child with Type 1 Diabetes. Insulearner Web is based on Cameron’s baseline algorithm and open-source software with additional improvements.
Insulearner uses a novel, data-driven approach for more personalized settings, leveraging first principles and modern machine learning techniques. It was created by Cameron Summers, a data scientist and dad of a child with Type 1 Diabetes. Insulearner Web is based on Cameron’s baseline algorithm and open-source software with additional improvements.
Data Sources: Insulearner Web connects with Tidepool, so a Tidepool account with up-to-date data is required. NOTE: This tool relies on carb counting for its calculations. You must count your carbs, or it will not work. PLEASE REMEMBER, this is experimental and may not be accurate or reliable.
Read more: Insulearner