In this week’s issue of The Savvy Diabetic:
-
-
- Abbott Issues Correction for Millions of Glucose Sensors
- Metformin Behaves Differently in Type 1 Diabetes
- Eli Lilly Becomes First Trillion-Dollar Health Company
- Diabetes and Associated Autoimmune Conditions You Need to Know About
- Survival of Transplanted Allogeneic Beta Cells with No Immunosuppression
- The Fastest Five Minutes with @ahncall with Neil Greathouse/@TheBetes
- UPDATE re Last Week’s Post about Stanford Study: Dan Heller Explains
- The Bad 1 | Silent Film | Spoonful of Laughter
- Does Eating More Protein Burn More Calories?
-
Abbott issues correction for millions of glucose sensors by Elise Reuter for MedTechDive.com, 24 November 2025.
 Abbott has issued a medical device correction for about 3 million Freestyle Libre 3 and 3 Plus sensors in the U.S. after determining that some sensors may provide incorrect low glucose readings. Abbott has received reports of 736 severe adverse events and seven deaths overall associated with the problem. In the U.S., 57 severe adverse events were reported, none resulting in death.
Abbott has issued a medical device correction for about 3 million Freestyle Libre 3 and 3 Plus sensors in the U.S. after determining that some sensors may provide incorrect low glucose readings. Abbott has received reports of 736 severe adverse events and seven deaths overall associated with the problem. In the U.S., 57 severe adverse events were reported, none resulting in death.
The problem could lead to incorrect treatment decisions, such as people skipping or delaying insulin doses and excessive carbohydrate intake. Abbott said it has resolved the issue, which was related to one production line, and will replace any potentially affected sensors at no charge. Abbott said it continues to produce Libre 3 and Libre 3 Plus sensors to fulfil replacement and new orders, and that it does not expect supply disruptions.
Read more: Abbott issues correction for millions of glucose sensors
Metformin Behaves Differently in Type 1 Diabetes by Rhianna-lily Smith for TechnologyNetworks.com, 27 November 2025.
 A new study from the Garvan Institute shows that Metformin behaves differently in type 1 diabetes (T1D) than many assumed. The trial found that metformin does not improve insulin resistance in adults with type 1 diabetes, but it does reduce the amount of insulin people need each day. For some, simply injecting insulin is not enough. Over time, the body’s tissues can become less responsive to insulin – a state known as insulin resistance. In T1D, insulin resistance has been recognized for years, yet the mechanisms underlying it remain unclear.
A new study from the Garvan Institute shows that Metformin behaves differently in type 1 diabetes (T1D) than many assumed. The trial found that metformin does not improve insulin resistance in adults with type 1 diabetes, but it does reduce the amount of insulin people need each day. For some, simply injecting insulin is not enough. Over time, the body’s tissues can become less responsive to insulin – a state known as insulin resistance. In T1D, insulin resistance has been recognized for years, yet the mechanisms underlying it remain unclear.
“Insulin resistance is a growing problem in T1D. Not only does it make regulating blood sugar levels difficult, but it is an underappreciated risk factor for heart disease, which is one of the biggest causes of health complications and deaths in those with T1D,” said lead author Dr. Jennifer Snaith, an endocrinologist and research fellow based at the Garvan Institute of Medical Research.
Metformin did not improve insulin resistance in any tissue. However, those taking metformin needed less insulin each day. “Although we didn’t find changes to insulin resistance from the use of metformin, we did show that people taking it used around 12% less insulin than those on placebo. This is an important result,” said Snaith. The trial also found higher levels of GDF15 in those taking metformin, a pattern seen in T2D research, along with a small drop in visceral fat that did not hold after further checks. Appetite and calorie intake remained unchanged, and metformin was well tolerated.
The findings indicate that although metformin should not be used to treat insulin resistance in adults with T1D, its insulin-sparing effect is still meaningful. Using less insulin can reduce day-to-day burden, and the long-term use of high insulin doses has been linked to insulin resistance. Cutting doses could lower cardiovascular risk. The work also suggests that metformin acts through a different route in T1D than in T2D. Current ideas now focus on the gut, including changes in gut bacteria and signals produced in the digestive tract. The rise in GDF15 seen in the study also fits these ideas. “There is increasing evidence suggesting that metformin may act on the gut. This is why we are now investigating how metformin changes gut flora, also known as the microbiome, in people with T1D. This has not been studied before in T1D,” said Snaith.
The number of participants was modest, and most had HbA1c levels below 9.5%, so people with poor glucose control were underrepresented.
Read more: Metformin Behaves Differently in Type 1 Diabetes
Eli Lilly Becomes First Trillion-Dollar Health Company by EndocrinologyAdvisor.com, 25 November 2025.
Eli Lilly reached a major milestone Friday, becoming the first healthcare company in the world to hit a $1 trillion market value. The drug company briefly crossed the trillion-dollar mark during morning trading before its stock pulled back slightly. Shares were last trading at around $1,048 each. Eli Lilly is now just the second non-technology company in the U.S. to reach a $1 trillion value, after Warren Buffett’s Berkshire Hathaway.
Much of that growth comes from two blockbuster drugs: Mounjaro for diabetes and Zepbound for weight loss. The Indianapolis-based drugmaker’s stock is up more than 36% this year, as demand for its weight loss and diabetes treatments continues to rise, CNBC reported. The company said Mounjaro brought in $6.52 billion in the third quarter, a 109% jump from the year before. At the same time, Zepbound generated $3.59 billion, up 184% compared to last year.
Eli Lilly expects to keep growing as more patients gain insurance coverage and new approvals expand access. The company also plans to release an oral version of its weight loss drug next year, which could make treatment easier for patients who don’t want a shot.
Read more: Eli Lilly Becomes First Trillion-Dollar Health Company
Diabetes and Associated Autoimmune Conditions You Need to Know About by Drs. Steve Edelman & Jeremy Pettus for TCOYD.org, 15 November 2025.
Dr Jeremy Pettus and Dr Steve Edelman shine a light on the most common ones that often appear with type 1 diabetes, why they occur in the first place, when you should be screened, and which subtle symptoms should raise a red flag.
They walk through what’s common but manageable, like thyroid issues and celiac disease — as well as what’s rare but critical not to miss, like Addison’s disease (adrenal failure), which can be dangerous if left undiagnosed but incredibly treatable once caught early. Most importantly, Jeremy and Steve explain how simple blood tests can detect these conditions before they spiral out of control, and how the right medication can completely change how you feel day to day. In this episode, you will explore:
-
-
-
- T1D & Autoimmunity 101: Why having one autoimmune condition raises your risk for others
Thyroid Disorders: The most common — hyper vs. hypo, yearly screening, easy treatment
Celiac Disease: Why it’s up to 10x more common in T1D and often missed without symptoms
Addison’s Disease Awareness: The “silent” cortisol deficiency you don’t want to miss
Proactive Care Mindset: How to build autoimmune screening into your diabetes warranty plan
- T1D & Autoimmunity 101: Why having one autoimmune condition raises your risk for others
-
-
Survival of Transplanted Allogeneic Beta Cells with No Immunosuppression, a new study published in the New England Journal of Medicine, 4 August 2025, as DOI: 10.1056/NEJMoa2503822
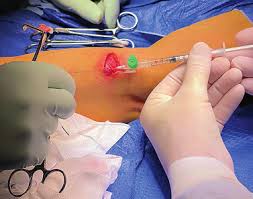 In a study by Per-Ola Carlsson, MD, et. al, suppressing a patient’s immune system after allogeneic cell transplantation is associated with wide-ranging side effects. We report the outcomes of transplantation of genetically modified allogeneic donor islet cells into a man with long-standing type 1 diabetes.
In a study by Per-Ola Carlsson, MD, et. al, suppressing a patient’s immune system after allogeneic cell transplantation is associated with wide-ranging side effects. We report the outcomes of transplantation of genetically modified allogeneic donor islet cells into a man with long-standing type 1 diabetes.
We used clustered regularly interspaced short palindromic repeats (CRISPR)–CRISPR-associated protein 12b (Cas12b) editing and lentiviral transduction to edit the cells to avoid rejection genetically; the cells were then transplanted into the participant’s forearm muscle. He did not receive any immunosuppressive drugs and, at 12 weeks after transplantation, showed no immune response against the gene-edited cells. C-peptide measurements showed stable and glucose-responsive insulin secretion.
Read more: Survival of Transplanted Allogeneic Beta Cells with No Immunosuppression (Requires subscription for full transcript)
The fastest five minutes with @ahncall … and he crushed it by TheBetes/Neil Greathouse on Instagram.com, 26 November 2025.
 I just love this short reel (the full episode will be released 12/1/25). The fastest five minutes with Dr. David Ahn (@ahncall). Short, honest and packed with things you can actually use. Thank you, Neil and David!!!
I just love this short reel (the full episode will be released 12/1/25). The fastest five minutes with Dr. David Ahn (@ahncall). Short, honest and packed with things you can actually use. Thank you, Neil and David!!!
Watch: The fastest five minutes with @ahncall
UPDATE re Last Week’s Post: Type 1 diabetes cured in mice with gentle blood stem-cell and pancreatic islet transplant
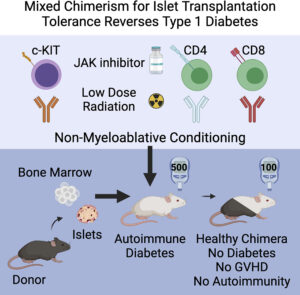 <<A combination blood stem cell and pancreatic islet cell transplant from an immunologically mismatched donor completely prevented or cured Type 1 diabetes in mice, according to a study by Stanford Medicine researchers. None of the animals developed graft-versus-host disease — in which the immune system arising from the donated blood stem cells attacks healthy tissue in the recipient — and the destruction of islet cells by the native host immune system was halted. After the transplants, the animals did not require immunosuppressive drugs or insulin for the duration of the six-month experiment.>>
<<A combination blood stem cell and pancreatic islet cell transplant from an immunologically mismatched donor completely prevented or cured Type 1 diabetes in mice, according to a study by Stanford Medicine researchers. None of the animals developed graft-versus-host disease — in which the immune system arising from the donated blood stem cells attacks healthy tissue in the recipient — and the destruction of islet cells by the native host immune system was halted. After the transplants, the animals did not require immunosuppressive drugs or insulin for the duration of the six-month experiment.>>
According to Dan Heller, the Stanford study about curing T1D mice is not what it seems. This is not really about curing T1D at all. It just so happens that diabetic mice are really good subjects for studying new approaches to treat autoimmune diseases. In this case, mostly lupus and others.
Read Dan’s explanation: Dan Heller Explains Stanford study
The Bad 1 | Silent Film | Spoonful of Laughter by DiaTribeNews.org, 14 November 2025.
Nothing says comedy like a dead pancreas.
The Bad 1, a Project Lemon Drop production by filmmaker and T1D Dad Jeff Bowser, takes a satirical swing at the stigma and outdated myths surrounding (type 1) diabetes, and the importance of human connection in combating them. Recognised as an Official Selection at CineHealth, an Official Selection at Awareness Festival, and awarded Best Low-Budget Film at Night of Shorts. In collaboration with Spoonful of Laughter, a diaTribe Foundation initiative to end diabetes stigma: https://spoonfuloflaughter.org/
Does Eating More Protein Burn More Calories? by Peter Attia for PeterAttiaMD.com, 1 November 2025.
Whether or not a calorie deficit is achieved is determined by the difference between total energy in and total energy out. Assessing the “energy in” side of the equation is straightforward—add up the energy content of all food consumed. However, the “energy out” side is more complex and much more challenging to measure accurately, as it varies with body composition, activity level, age, sex, and other factors.
One component of total daily energy expenditure (TDEE) is the energy required to digest and metabolize food, known as the “thermic effect of food” or “diet-induced thermogenesis” (DIT). DIT can account for ~10% of total energy expenditure, but some foods require greater energy input for digestion and metabolism than others. Among macronutrients, protein is by far the least efficient source of energy—roughly 25% of the available energy in protein is expended just metabolizing it, which is more than double the amount of available energy required by carbohydrate, fat, or alcohol metabolism.
It has been repeatedly demonstrated that higher-protein diets are superior for producing sustained fat loss and maintaining lean mass. High-protein diets affect both sides of the energy balance equation. Protein has a substantially more substantial anorexic effect than other macronutrients and can thus promote a reduction in energy consumption, and this satiating effect of dietary protein likely has a greater impact on the relationship between protein intake and fat loss than the relatively small increase in energy expenditure.
Read more: Does eating more protein burn more calories?

